CC: Shortness of Breath
HPI: ALS box call to St. Joseph Wayne ED # 1: 92 year old female from nursing home with PMH of Alzheimer Disease and failure to thrive, RUE DVT on Eliquis with complaints of SOB. BiPAP was initiated in the nursing home with minimal improvement. On arrival, Patient was in severe respiratory distress, tripoding and with an O2 saturation of 75% on BiPAP. Patient was tachycardic with initial HR of 130bpm, BP 100/80 with a RR of 30.
Med control: Intubation was advised with 50 mcg of Fentanyl, 18 mg of Etomidate, 75 mg of Succinylcholine, and 1 mg of Ativan for post-intubation sedation. NS IV Fluids were started and patient was to be transported to PCI Center St. Joseph Regional Center Paterson for Cardiac catheterization.
ALS box call to St. Joseph Wayne (SJW) ED #2: Patient los pulses after intubation. CPR was in progress.
Med control: Transfer to SJW, continue ACLS
Patient arrives in SJW with return of spontaneous circulation (ROSC) status-post Epinephrine x 2 and total CPR time 3-4 minutes.
Physical Exam:
Palpable Carotid Pulses. Endotracheal Tube (ETT) was confirmed
BP 81 / 68 HR140 RR20 T: 96.5 F SaO2 94%.
Intubated, GCS 3T, Pupils 4mm equal and reactive bilaterally
Respiratory exam: Equal but diminished breath sounds throughout.
GI: Abdomen soft
Extremities: 2+ femoral pulses B/L, no peripheral edema.
Pertinent Labs (if any):
Na: 138 K: 3.7 CL: 116 CO2: 10 BUN: 37 Cr: 1.14 Platelet: 195
WBC: 10 Hg: 6.6 Platelet: 265
INR 6.3
ABG: 7.17/28/62/11
UA: nitrite +, large LE, WBC 6-10, Moderate bacteria, Large blood, RBC TNTC
Troponin: 0.042
Lactic Acid: 6.3
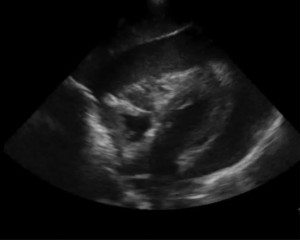
Pertinent Imaging/EKG: Bedside Cardiac Echocardiogram: Severe pericardial effusion with diastolic RV collapse.
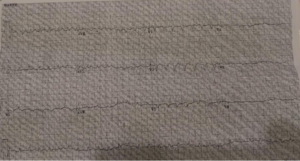
Initial EKG post intervention: Sinus tachycardia, low voltage
Working Diagnosis at time of Disposition: Urinary Tract Infection and Pneumonia with Sepsis
Acute Respiratory Failure
Cardiac Arrest with ROSC
Cardiac Tamponade, possibly iatrogenic
Supratherapeutic INR
ED/Hospital course:
A blind subxiphoid pericardiocentesis was performed. 50cc of frank blood was aspirated and no coagulation of aspirate was noted. Repeat vitals signs were BP 94 /74; Pulse 103; RR 20; Pulse Ox 98%.
Ultrasound was used to confirm the presence of the guide wire in the pericardial space. A triple lumen was passed over the guide wire and secured into placed. A total of 350cc was aspirated with repeat vitals: BP 111/73; Pulse 74; RR 20; Temp 97.6; Pulse Ox 99%.
A subclavian triple lumen catheter was placed and patient was given 2 PRBCs, 2 FFPs, 10mg IV Vitamin K, and 1L NS. Cardiologist from St. Joseph in Paterson was called and he accepted the transferred to their CCU. Patient was started on Fentanyl and Ativan Drip. Levophed gtt was also started for transport.
While in the CCU, patient was continued on antibiotics and vasopressors for septic shock.
Cardiac ECHO showed LV EF 65 to 70%, impaired relaxation pattern of LV diastolic filling, moderate concentric LVH, moderate pericardial effusion is present, no hemodynamic compromise, echogenic material adherent to the visceral pericardium, especially anteriorly measuring approximately 0.5 cm in thickness.
On Hospital day 2 (HOD), Cardiothoracic was consulted. They determined “patient currently very ill and unable to tolerate OR. Not stable for OR at this time.” Pericardial fluid was sent for evaluation.
Pericardial fluid results: Exudative as LDH 1613 with RBC count 1 million; ANA positive, RF negative.
Patient was additionally seen by palliative care. It was also determined there was no surgical interventions needed for the effusion. Sputum culture grew MRSA.
On Hospital day #4, Patient was following commands and was taken off the vasopressors. She self extubated and failed a trial on BiPAP and was re-intubated.
Patient was extubated on HOD #9 and discharged back to Nursing Home on HOD#15.
EKG post ER interventions: NSR, improved amplitude, prolonged QT

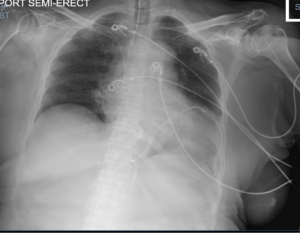
CXR post procedure: Enlarged heart, LLL infiltrate with obscured L hemi-diaphragm, ETT above carina, R subclavian central line, Pericardardial drain
| Pearls & Takeaways | · Tamponade:
o Obstructive shock from impaired cardiac filling due to pericardial accumulation o As fluid accumulates, pericardial pressure become greater than the cardiac relaxing pressures o Incidence 2/10,000 in USA. o TB #1 cause in developing countries. Viral and postsurgical complications #1 cause in developed countries. Differential includes malignancy, infectious including HIV, idiopathic, atrogenic, trauma, uremia, hypothyroid, rheumatologic, and post radiation. o Symptom development depends on rate of fluid accumulation and amount. Pericardial compliance accommodates a slower rate of volume expansion. o Signs include persistent tachycardia, JVD, muffled heart sounds, pericardial friction rub, hepatomegaly, peripheral edema, pulsus paradoxus. Hypotension and bradycardia precede cardiac arrest. o Pulsus paradoxus reportedly present in 98% of tamponade cases even prior to onset of hypotension. o Pulsus paradoxus (decrease in SBP >10% during inspiration) occurs because the negative intrathoracic pressure during inspiration increases venous return and pulmonary vasculature compliance with subsequent pulmonary vascular pooling. RV engorges with septal shift causing decreased LV filling, SV, and SBP. o Pulsus paradoxus can be seen on plethysmogram. 1998 study by Frey of 57 PICU patients shows sensitivity of 89% and specificity of 90% to detect pulsus paradoxus 10% change with a pleth variation of 8mm. o EKG findings include low voltage, tachycardia, electrical alternans, PR depression, nonspecific ST/T changes o CXR may show enlarged silhouette o Bedside ECHO § Effusion · Trivial is seen only in systole · Mild < 10mm · Moderate 10-20mm · Severe >20mm § Collapse of chambers during relaxation · Atrial collapse precedes ventricular collapse · Atrial collapse longer than 1/3 of cardiac cycle has 100% sensitivity and specificity of tamponade · M Mode with EKG tracing through collapsing wall · RV indentation is more sensitive and specific than pulsus paradoxus § IVC size > 20mm is 92% sensitive · Pericardiocentesis: Indicated when hemodynamic compromise is present § US may guide you if necessary: if only RA collapse and RV unaffected, may wait to CTS consult o Needle aspiration with drain placement for repeat aspiration if re-accumulation occurs § Triple lumen catheter is most readily available in the ER though CTS prefers pigtail catheters due to decreased clotting o Subxiphoid approach (blind or US guided) § Insert needle at xiphoid process at 45 degree angle and aim towards tip of left scapula/left areola. Advance slowly until fluid aspirated. § US guided may be limited by habitus. Needle will enter pericardium inferior to the RV. o Parasternal (US) § Probe on left parasternal position at 4th intercostal space (Long axis view). Needle should be inserted in-plane with probe at a 45 degree angle. Will enter pericardial space anterior to RV. § Preferred over subxiphoid due to closer proximity to effusion and better ability to avoid liver and lung o Confirmation § Aspirated blood should not clot due to anticoagulative factors in space § Agitated saline flush showing “snow-storm appearance” § Repeat vitals after aspiration o Complications § PTX § Myocardial, coronary artery injury § Arrhythmias § Cardiac arrest § Liver injury |
Case presented by Nick