Written by Amanda Hall, DO
This post first appeared on REBEL EM
Background: Epistaxis is a common ailment experienced by millions worldwide. While most of these cases can be managed by patients at home, some will require medical attention. Initial interventions include local pressure, ice, and forward head positioning for persistent bleeds. When simple maneuvers fail, we proceed to topical agents such as lidocaine with epinephrine, oxymetazoline, anterior nasal packing, and electrical or chemical cauterization.
Tranexamic acid (TXA) is an antifibrinolytic drug that inhibits the enzymatic breakdown of fibrin blood clots. Essentially, it increases blood clot stability. TXA has been studied extensively over the last 10 years for various conditions, including trauma, hemophilia, bleeding related to pregnancy, and other uncontrolled bleeding. However, the benefit vs. harm of using TXA topically for epistaxis is unclear.
TXA has become the standard practice in the ED based on small RCTs, though larger trials have not demonstrated the same benefit (REBEL EM review). Here, we explore one of the original trials which formed the basis of care and moved TXA into standard practice.
Paper: Zahed R, Moharamzadeh P, Alizadeharasi S et al. A new and rapid method for epistaxis treatment using injectable form of tranexamic acid topically: a randomized controlled trial. Am J Emerg Med. 2013 Sep;31(9):1389-92. Epub 2013 Jul 30. PMID: 23911102.
Clinical Question: Does the topical application of standard injectable tranexamic acid in adult patients presenting to the ED with persistent epistaxis reduce the need for anterior nasal packing?
What They Did:
- ED-based unblinded randomized clinical trial at a single center in Iran
Population:
- Inclusion criteria: Patients with idiopathic anterior epistaxis
- Exclusion criteria: Major trauma, posterior epistaxis, bleeding disorder (thrombocytopenia, hemophilia, platelet disorders), INR greater than 1.5, shock, visible bleeding vessel
Intervention:
- Patients with idiopathic anterior epistaxis were randomly assigned on a 1:1 basis to either:
- Arm 1: TXA (500 mg in 5 ml), soaked cotton pledget inserted into the bleeding nostril
- Arm 2: 2% Lidocaine with epinephrine, soaked cotton pledget placed in bleeding nostril for 10 minutes, then anterior nasal packing applied, with several cotton pledgets covered with tetracycline
Outcomes:
- Frequency of patients for whom bleeding arrested within 10 minutes from treatment onset
- Rebleeding within 24 hours, and within 7 days
- Hours of stay in ED
- Patient satisfaction, evaluated on a 0-10 scale
Results:
- 316 were assessed for eligibility
- 216 were randomized, 107 to TXA and 109 to anterior nasal packing
- No patients were lost to follow-up
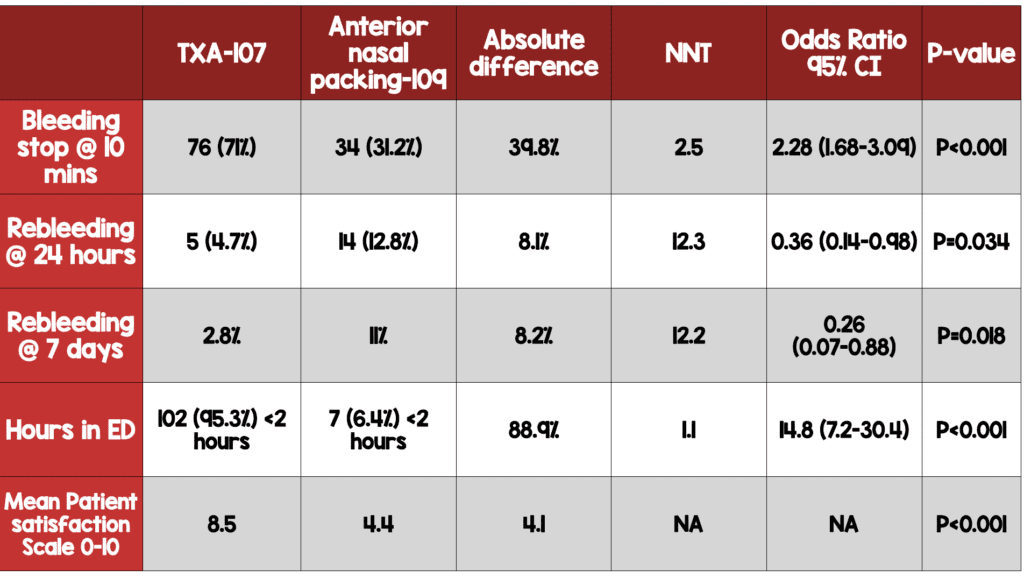
- TXA showed superiority to anterior nasal packing in all five efficacy variables, as shown in the table. These findings were statistically significant in each case.
Adverse Effects:
- No serious adverse events were noted.
- 11% of patients in the anterior nasal packing arm and 4.7% of patients in the TXA arm were noted to have complications in the ED, but this difference was not statistically significant (P = 0.128)
Strengths:
- Outcomes are all patient-oriented
- Pragmatic study, which is broadly applicable
- Looked at patient satisfaction, which is important to consider in compliance
- Few adverse outcomes
Limitations:
- Small, single-center study in Iran, which affects generalizability and applicability.
- Non-consecutive enrollment leads to selection bias
- The primary outcome was not explicitly stated
- 100 patients were excluded for unclear reasons
- There is no discussion of treatments attempted prior to the application of TXA
- There is no control arm for comparison
- Patient characteristics showed 58.1% of the TXA arm had a history of prior epistaxis, compared to 13.6% of the anterior nasal packing arm; this could indicate a bias with the randomization process.
- Patients and physicians were unblinded, leading to a potential for significant bias
- Patients on antiplatelet and anticoagulant medications are a large percentage of patients who present with epistaxis, so it will be difficult to know how this study will apply to them.
Discussion:
- Patients were randomized by simple randomization generated by SPSS software. Medications and cotton pledgets for each arm were packed in blinded boxes by a research nurse outside the ED. However, since the respective medications had very different consistency, color and smell, and the two arms used different numbers of pledgets, the physicians and patients were not truly blinded. This could introduce bias into decisions by the physicians about management and discharge. The data analysts, however, were blinded to the group assignments.
- The primary outcome of cessation of bleeding is somewhat subjective, and therefore implicit bias could have occurred if the researchers believed TXA to be the better treatment option. Their knowledge of group assignments could influence their assessments.
- TXA has been utilized for a variety of reasons in medicine; due to this trial TXA was used by providers for nearly a decade to aid in the care of patients with epistaxis. While this study has some flaws, the efficacy and lack of adverse outcomes demonstrated this paper made many providers jump at the opportunity to assist these patients and avoid the discomfort associated with anterior nasal packing.
- As TXA appears to have good efficacy for anterior nosebleeds, with few adverse effects, it could be a good modality to use to avoid anterior nasal packing; however, larger studies should be performed.
- These authors performed an additional study in 2018, “Topical TXA Vs. Anterior Nasal Packing In Epistaxis With Antiplatelet Drugs” (3) which looked specifically at patients on antiplatelet medications. Patients in this study received 20 minutes of manual pressure and then were randomized to TXA or anterior nasal packing. This study also found in favor of TXA for bleeding cessation at 10 minutes, 73% with TXA compared to 29% with nasal packing.
- The NoPAC trial, which was published in 2021,(1) compared TXA to placebo in a large multicenter randomized control trial in the UK which looked at data from 26 emergency departments. The primary outcome was the need for anterior nasal packing and they found that 43.7% in the TXA group versus 41.3% in the placebo group required nasal packing. This difference was not statistically significant.
- The systematic review and meta-analysis by Janapala et al (2) was performed in April of 2021 and concluded that TXA is beneficial in the cessation of epistaxis. The authors found that patients were 3.5 times more likely to have cessation of bleeding at the first reassessment after application of TXA, and additionally the rate of return to the ED was lower. The NOPAC data was not included in this meta-analysis because that study did not measure time to bleeding cessation or bleeding recurrence.
Authors’ Conclusions: “The results of this trial showed that treating anterior epistaxis with the topical use of injectable form of tranexamic acid is better than usual nasal packing. ”
Our Conclusions: The authors claim superiority of topical TXA compared to anterior nasal packing for treating idiopathic anterior epistaxis. However, due to flaws in the study design, it is difficult to reach firm conclusions. Furthermore, findings in the more recent NoPAC trial contradict the authors’ conclusions. Nonetheless, TXA is an inexpensive medication with few adverse effects, so although more extensive better-designed studies are needed, we should consider it a potential modality in uncontrolled epistaxis.
Read More:
- REBEL EM: The NoPAC Trial – TXA for Epistaxis?
- REBEL EM: Meta-Analysis on Topical TXA for Epistaxis
- EMRAP: EMA review of this article (2014)
- EMRAP: EMA TXA vs anterior packing in patients taking anti platelets (2018)
- EMRAP: EMA NoPAC (2021)
References:
- Reuben A, Appelboam A, Stevens KN, et al. The Use of Tranexamic Acid to Reduce the Need for Nasal Packing in Epistaxis (NoPAC): Randomized Controlled Trial. Ann Emerg Med. 2021;77(6):631-640. PMID: 33612282
- Janapala RN, Tran QK, Patel J, Mehta E, Pourmand A. Efficacy of topical tranexamic acid in epistaxis: A systematic review and meta-analysis. Am J Emerg Med. 2022;51:169-175. PMID: 34763235
- Zahed R, Mousavi Jazayeri MH, Naderi A, Naderpour Z, Saeedi M. Topical Tranexamic Acid Compared With Anterior Nasal Packing for Treatment of Epistaxis in Patients Taking Antiplatelet Drugs: Randomized Controlled Trial. Acad Emerg M2018;25(3):261-266. PMID: 29125679

PGY-2, Emergency Medicine Resident
Saint Joseph’s University Medical Center, Paterson New Jersey
Email: [email protected]
Associate Professor, Emergency Medicine
Saint Joseph’s University Medical Center, Paterson New Jersey
Twitter: @hochmast

Vice-Chair, Emergency Medicine
Vassar Brothers Hospital, Poughkeepsie New York
Twitter: @marco_propersi
Post-Peer Reviewed By: Anand Swaminathan, MD (Twitter: @EMSwami) and Salim R. Rezaie, MD (Twitter: @srrezaie)