| Brief HPI |
30-year-old male with no past medical history presented with acute onset left ocular pain and double vision x1d. Patient states that last night he turned off the light and had immediate symptoms. Patient denies using glasses or contact lenses. Patient has never felt this before. Patient has not taken anything for the symptoms. No primary care physician. Denies any associated fever, chills, blurry vision, redness of the eye, discharge from the eye, nausea or vomiting, focal weakness, dysphagia, dysarthria, parasthesias, sob, chest pain, cough, abd pain, trauma. |
| Pertinent PE and Vitals |
T: 36.4 °C HR: 86 RR: 20 BP: 146/79 SpO2: 98%
Constitutional: Alert, awake, comfortable
Head/Face: Normocephalic, atraumatic, no temporal artery tenderness
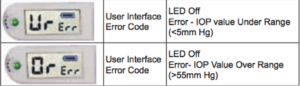
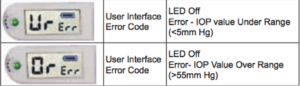
Eye: OD 2 mm reactive, OS 6 mm nonreactive; APD present; EOMI, no nystagmus; intraocular pressure OD 21, OS error ×3; acuity OD 20/20, OS 20/40
ENT: Moist mucous membranes; Posterior Pharynx is without erythema and exudates, Airway is patent
Neck: ROM is full and without pain, no spinous process tenderness, trachea midline
Cardiovascular: Regular rate, regular rhythm, S1, S2, no murmurs, gallops, or rubs
Respiratory: No respiratory distress, breath sounds are equal bilaterally, no rales, no rhonchi, no wheezing.
Abdomen/Gi: Appears normal, Bowel Sounds present; Soft, non-tender, no guarding or rigidity.
Neuro: Oriented to person, place and time, Lucid thought process, follows commands. Strength 5/5 all extremities, Sensation intact, cerebellar signs absent
Musculoskeletal: Full active ROM without pain, 2+ b/l DP, PT.
Skin: Warm, dry, no rash or injuries |
| Pearls & Takeaways |
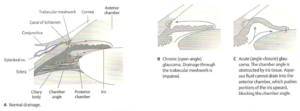
Ø Glaucoma is characterized by increased intraocular pressure which will compress the optic nerve and can cause vision disturbances and, if left untreated, blindness.
Ø Aqueous humor normally drains from the posterior chamber, through the iris/lens interface into the anterior chamber, through the trabecular meshwork and out through the canal of Schlemm and into the episcleral vein.
Individuals with shallow anterior chambers are more susceptible to closure of the angle because the iris and lens have a greater area of contact with subsequent bowing of the iris, blocking drainage.
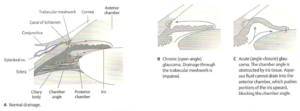
Ø Acute angle closure attacks are mostly precipitated by pupillary dilation, increased iris/lens contact, blocked aqueous flow into the anterior chamber and increased posterior chamber pressure that causes worsening bowing or the iris against the canal.
o Pupillary dilators: dim light, mydriatics, antihistamines, anticholinergics, TCAs, adrenergics, emotional stress, antiparkinsonians
Ø Far-sightedness is a risk factor due to anatomic flatter corneas, narrower angles, and shorter Anterior to Posterior lengths.
Ø Family history, Asian descent, female, age (lenses thicken and anterior chambers narrow) are additional risk factors
Ø The increase in IOP will cause corneal edema and cause the cornea to appear hazy and the patient to complain of blurred vision and/or halos.
Ø Conjunctival injection, mid-dilated (5-6mm) pupil, hardness of globe (may use contralateral eye or nose as reference), decreased acuity are some exam findings
Ø Fundoscopic exams are more difficult due to corneal edema but may show a pale, cupped optic disc with cup-to-disc ration > 0.6
Ø Slit lamp will show shallow anterior chamber and corneal cloudiness
Ø Oblique flashlight test: if shadow appears on nasal iris when penlight shone from temporal side with beam parallel to iris angle is narrow (sensitivity 76%, specificity 81%)
Ø IOP > 22 is hallmark.
o Tonopen: Be kind and anesthetize the eye. Instruct patient to look straight ahead. Contact cornea for 10 applanations; you do not need to indent the cornea and it may lead to incorrect readings and corneal injury. Error codes are displayed. Two numbers will appear: the first is the IOP measurement and the second (smaller) number is the statistical confidence indicator (95 is acceptable, repeat if 80 or 80-). Tonopen tip should be cleaned with canned air for 3 seconds and should occur monthly if 10 pts/week.
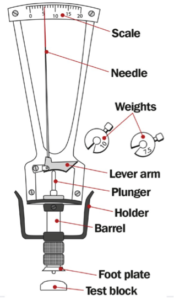
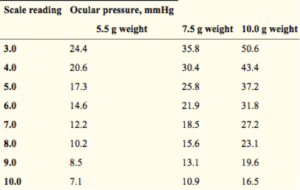
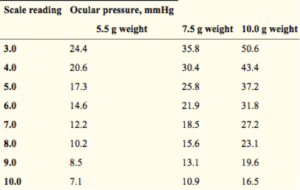
o Shiotz: Measures via indentation tonometry and is dependent upon scleral rigidity.
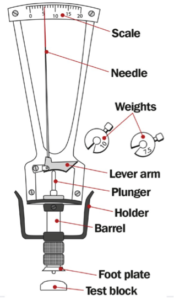 
§ Check calibration by testing tonometer against spherical mould and 5.5g weight: pointer should read 0.
§ Clean, anesthetize, have patient look straight at fixed point (their own outstretched finger)
§ With 5.5g weight, gently lower tonometer disc onto corneal surface and note reading.
§ If 2 or less, replace weight with 7.5g weight and repeat. If again 2 or less, use 10g weight.
o Goldmann applanation: gold standard
 
§ Calibrate with the dial at 0mmHg, insert control weight. Set measuring drum at 0mmHg. If prism does not tilt forward and backward with the turning of the measuring drum up to +2 and -2, then calibration required. (Beyond the scope of this review)
§ Anesthetize and instill fluorescein, dab the eyes dry.
§ Patient positions into slit lamp with eyes level with black alignment marker
§ Maximum brightness of light
§ Blue light
§ Touch central surface of cornea with prism and then pull back
§ View cornea through miscroscope. 2 semicircular rings (mires) will be seen.
§ Adjust drum until mires line up. IOP is 10x the drum reading.
Ø TREATMENT: should be in co-ordination with specialist but based on following principle:
o Decrease production
§ Topical Beta-blocker: timolol 0.5% 3 drops q15m x3
§ Topical alpha-2 agonist: brimonidine 0.15% or apraclonidine 1% 3 drops q15m x3
§ Topical CA inhibitor: dorzolamide 2% 3 drops q15m x3
§ Systemic CA inhibitor: acetazolamide 500mg IV/PO
§ Topical anti-inflammatory: prednisolone acetate 1%
o Increase drainage
§ Topical prostaglandin: latanoprost 0.005%
§ Systemic diuretic: mannitol 50g IV
§ Topical muscarinic (miotic): pilocarpine 1-2%
§ Surgical iridotomy (YAG laser typically) is typically curative if done early
References
· Cordero I. Understanding and caring for a Schiotz tonometer. Community Eye Health. 2014;27(87):57.
· Stevens S. How to measure intraocular pressure: Schiötz tonometry. Community Eye Health. 2008;21(66):34.
· TonoPen Avia User Guide. http://doclibrary.com/MSC167/PRM/68E3892-Rev-J-UG-AVIA4540.pdf
· Shikino K, Hirose Y, Ikusaka M. Oblique Flashlight Test: Lighting Up Acute Angle-Closure Glaucoma. Journal of General Internal Medicine. 2016;31(12):1538. doi:10.1007/s11606-016-3737-8.
· Chang DF. Chapter 2. Ophthalmologic Examination. In: Riordan-Eva P, Cunningham ET, Jr. eds. Vaughan & Asbury’s General Ophthalmology, 18e New York, NY: McGraw-Hill; 2011. http://accessmedicine.mhmedical.com/content.aspx?bookid=387§ionid=40229319. Accessed September 08, 2018.
· Laser iridotomy. http://www.littlerockeye.com/laser-iridotomy/
· Murphy-Crews, M. 2017. Angle Closure Glaucoma. Taming the Sru. http://www.tamingthesru.com/blog/annals-of-b-pod/b-pod-case/angle-closure-glaucoma
|