Source: EM Practice Podcast – Dec 2017
** There are no existing ACEP guidelines on this topic.
Pre-Hospital Management
- Stabilizing and pain control
- Neurovascular compromise
- If suspected then d/w med control for considerate of immediate reduction and splinting vs. rapid transport to ED
- If no suspicion the patient can be immobilized in current position
- Don’t forget C-spine precautions as these injuries are often distracting
Overview
Etiology:
- Typically traumatic in origin
- Over 2/3 Hip dislocations occur in patients who present after MVCs without seat belts with the knee hitting the dashboard and the body moving forward over a fixed femur.
- Often associated with posterior wall/lip fractures of the acetabulum
Definitions:
- Simple vs. Complex
- Simple Dislocation – does not involve fracture
- Complex Dislocation – involves fracture
Pathophysiology:
- Posterior & Inferior dislocations are most common – about 90% of dislocations
- Fracture of >40% of the acetabular rim is considered an UNSTABLE FRACTURE (requires ORIF)
- If there is a posterior acetabular fracture you must get a CT to eval for unstable fractures
- Sciatic nerve injury
- Seen in about 14% of traumatic hip dislocations
- Check sensory along the posterior leg, ability to dorsiflex the ankle and ankle reflexes
- 95% of traumatic hip dislocations will have another associated injury
- Be sure to complete a full trauma survey on these patients per ATLS guidelines
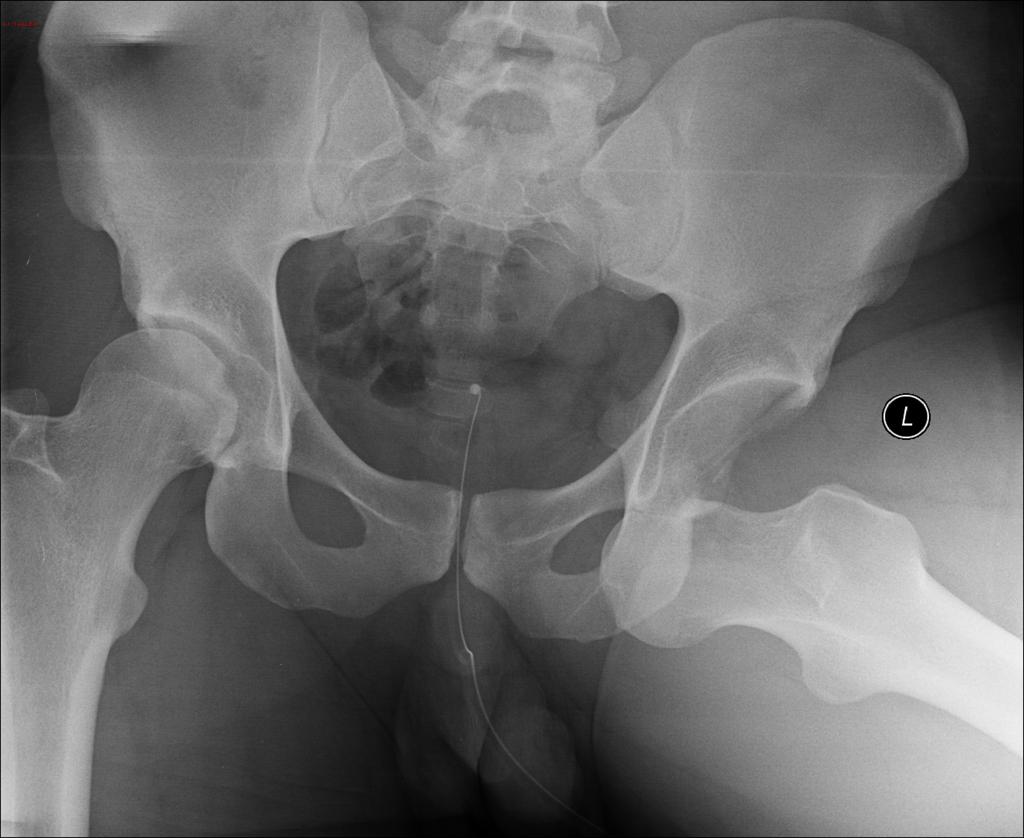
Imaging
- Initial image should be a bedside AP pelvic radiograph
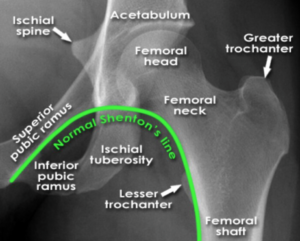
- Look for Shenton’s Line
- Lateral film can seal the diagnosis if unsure based on initial bedside AP
- CT if neeeded
Treatment for Native Hips (non-prosthetic)
Consultation
- Ortho Consultation are required for the following:
- Complex hip dislocations
- Irreducible dislocations
- Non-concentric reductions
- Neurovascular deficits despite reduction
Reductions
Who:
– Simple dislocations can & should be reduced by the ED physician!
When:
– Reduction should be performed within 6 hours of injury to decrease risk of avascular necrosis
– No more than 3 attempts at reduction should be made by the ED provider
Transfers:
– If patient requires transfer to a different hospital, an attempt at reduction should be made by the ED provider.
– Patients transferred without reduction had a 4-fold risk of severe sciatic nerve compared to those transferred after reduction (16% vs 4%).
Analgesia:
– Be sure pain is controlled prior to attempting reduction
- Ultrasound guided fascia iliaca compartmental block work great
- Reduces need for systemic analgesics
- Improves patient comfort
- Increases likelihood of successful reduction
- Reduce need for procedural sedation
- Be sure to have completed a full neurological exam prior to blocking your patient
LINK TO VIDEO
- In many cases, procedural sedation and systemic analgesia may also be needed (in addition to nerve block) in order to adequate pain control and muscle relaxation.
Reduction Techniques
Old School:
Allis’s Maneuver
Newer techniques:
Captain Morgan
Over-Under/Whistler
East Baltimore Lift
No evidence exists to recommend one technique over the other.
Immobilization
After successful reduction the hip should be immobilized in extension and external rotation with slight abduction
– Use an abduction pillow to help hold this position
– Knee immobilizer can be used if no abduction pillow is available
Don’t forget to obtain a post reduction film to confirm alignment
Other Recommendations
– Early passive range of motion and rehab is usually recommended
– Patients should remain non-weight bearing until seen by orthopedic services.
Notes on Prosthetic Hip Dislocations
- Quite common
- Incidence of ~2% of patients who undergo THA
- 60% occur within first 3 mo, 77% occur within the first year
- Often the result of minimal force like bending over to pick something up off the floor
- Use the same techniques as a native hip reduction
- Do not need abduction bracing after the reduction
- If the patient can walk after the reduction, they can be safely discharged (after discussion with their orthopedist)
- Less urgency, no risk of avascular necrosis as the femoral head has already been replaced
- Remember, these injuries are painful and although less urgent, the reduction should occur as soon as possible