Point-of-Care Ultrasound (POCUS) in Detecting Aortic Aneurysms
By: Dr. Shani Tal & Dr. Doris Ilic
Faculty Reviewer: Dr. Nicole Yuzuk
Case Presentation:
A 68-year-old female with past medical history significant for hypertension, hypothyroidism, congestive heart failure, hyperlipidemia, and chronic kidney disease presented to the Emergency Department (ED) complaining of worsening left sided flank pain radiating to the left side of her abdomen that started one day prior. She also reported associated fatigue with increased urination but denied dysuria or hematuria. She did not take any medication at home for pain relief. Of note, she had been admitted to the cardiac critical care unit (CCU) several times for hypertensive emergencies, but stated she was compliant with her antihypertensives. She denied fevers, chest pain, shortness of breath, nausea, vomiting or any other complaints.
On her arrival to the ED bed, she was found to be alert and oriented x3, however she was hypertensive with a systolic blood pressure in the 240s with all other vitals within normal limits. On physical exam, she appeared uncomfortable secondary to pain. She was noted to have positive CVA tenderness to the left flank and mild tenderness to the left abdomen. She did not have any obvious masses, distention, rebound or guarding.
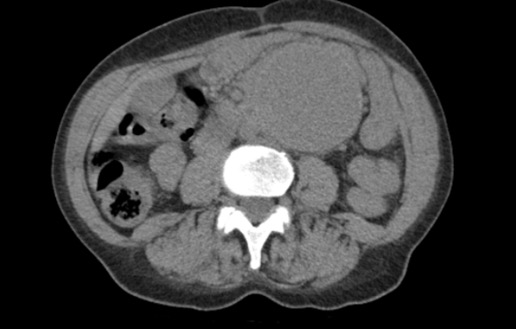
While in triage the screening nurse practitioner ordered labs and a CT abdomen/pelvis without contrast with concerns of possible kidney stone. Labs were significant for elevated creatinine of 3 (which was patient’s baseline), but otherwise no leukocytosis, anemia, or electrolyte abnormalities were noted. The CT scan ordered from triage (pictured below) was concerning for an abdominal aortic aneurysm (AAA), and ultrasound quickly performed bedside confirmed large infrarenal aneurysm (FAST negative).

Background:
Aortic pathologies are one of the most life-threatening emergencies that present to the Emergency Department. The aorta is comprised of three walls, the intima, media, and adventitia. An aneurysm forms when there is weakening of one of the walls causing a localized enlargement of the vessel. There are two types of aortic aneurysms: thoracic and abdominal. Abdominal aortic aneurysms are associated with atherosclerosis and risk factors include smoking, male sex, increased age, and family history. Their most common location is infrarenal. Thoracic aortic aneurysms are associated with cystic medial degeneration and tend to be associated with connective tissue disorders, HTN, bicuspid aortic valve and tertiary syphilis. Aortic aneurysms are of concern because as they enlarge, they risk further complications such as dissection or rupture.
There are different imaging modalities that can be used to identify an aortic aneurysm which includes CT scan, specifically CT angiography (CTA), and ultrasound. While CT tends to be the gold standard in most abdominal pathologies, ultrasound is the best initial diagnostic modality to identify an abdominal aneurysm as it is quick, painless, and without radiation exposure. The goal is to identify if the aorta looks enlarged as management changes based on the size of the aneurysm. Typically, if the aorta measures greater than 3 cm it is considered aneurysmal and if greater than 5 cm or concern for rupture immediate surgical consult is advised (1).
There is extensive literature published regarding the importance of using ultrasound to screen for AAAs especially for those with risk factors. Current guidelines recommend a one-time screening with ultrasonography for AAA in men who are 65-75 years of age and have a smoking history (2). Ultrasound is the best screening method not only because it is noninvasive and fast, but because it has a sensitivity of 94-100% and specificity of 98-100% for detecting AAA (9). Its high accuracy makes it beneficial to use for patients presenting to the emergency department with symptoms such as abdominal pain, back pain, flank pain, syncope, and shock.
Scanning technique and Sonographic findings:
The proper technique for scanning the aorta begins with proper patient position and probe selection. The patient should be laying supine for optimal views. The curvilinear probe is best used because of its ability to view deeper organs in adult patients. The abdominal aorta runs throughout the entire abdomen and has multiple views that are necessary to identify including the proximal, mid, and distal aorta. To begin finding the proximal aorta, place the probe in the subxiphoid region in a transverse orientation with the probe indicator to the patient’s right. The key landmarks to identify in this view include the vertebral body shadow which should allow you to identify IVC and aorta directly anterior, with IVC on the left and aorta on the right (See below, 8).
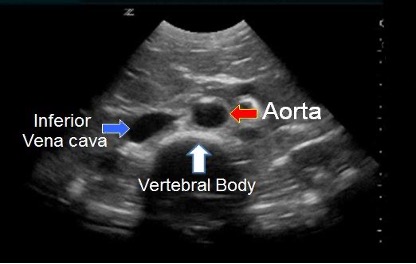
Reference: Core EM
To obtain all necessary views of the abdominal aorta, the abdomen should be scanned in the transverse plane from xiphoid process to the umbilicus.
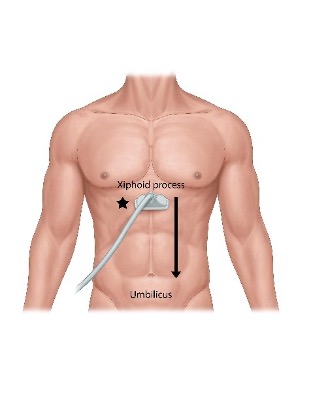
Reference: ACEP sonoguide aorta
- The first view to identify would be the proximal aorta, which is where you look for the classic “Seagull Sign.” In this view, you are looking for the celiac trunk and you should see the wings of the hepatic and splenic arteries branching off (See below).
Reference: Ali EM
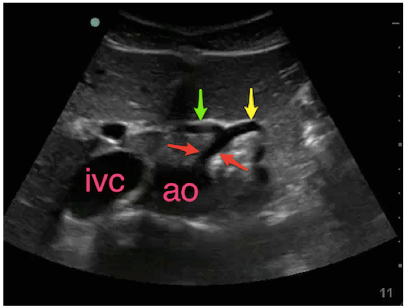
- To identify the mid aorta, you should look for the SMA which is the second branch of the abdominal aorta. The classic sign to see here is the “Mantle Clock Sign”. In this view you should see the splenic vein anterior and the left renal vein running posterior to the SMA (See below).
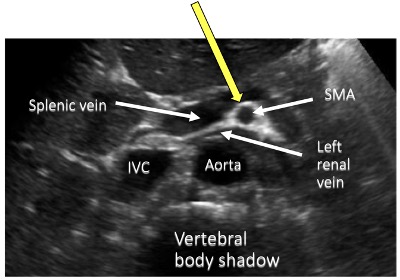
Reference: Ultrasound Guide
- To identify the distal aorta, you should look for the bifurcation around the level of the umbilicus, at L4. The aorta will branch into the common iliac arteries. To see the branches of the iliac artery coming off the aorta, slowly fan the probe up and down (See below).

Reference: Radiology Key
- The final view of the abdominal aorta is visualizing the aorta in long axis. This helps identify saccular aneurysms, when the outpouching/enlargement is only on one side of the vessel.
Case ultrasound findings:
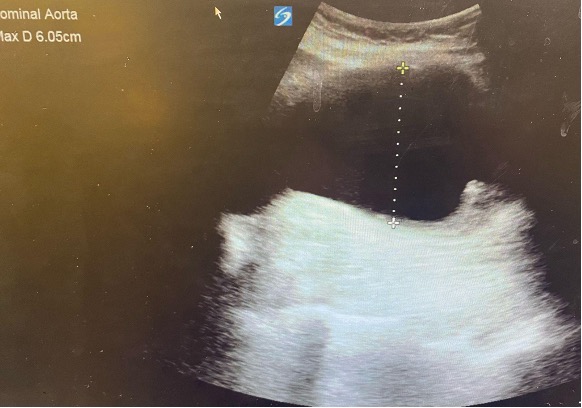
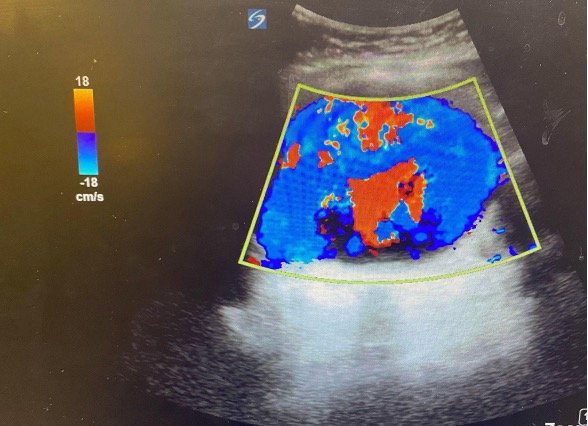
Using the techniques that were described above, the patient’s abdominal aorta was identified and was measured to be > 6 cm (see above image). The landmarks that are usually used to identify proximal, mid, and distal aorta were difficult to see on ultrasound due to the sheer size of the patient’s aneurysm. Color flow was used to confirm that what we were viewing was in fact vessel.
Conclusion:
There is lots of data proving the integral use of ultrasound in detecting aortic aneurysms. While CTA remains the gold standard for assessing for AAA and whether rupture has occurred, the use of ultrasound at bedside can expedite patient care and confirm your diagnosis while waiting for further testing. With its high sensitivity/specificity and quick results, we should be using POCUS to assess for AAA to treat the patient appropriately and avoid delay in patient care while waiting for the CTA.
Case Resolution:
Vascular surgery was consulted immediately after viewing the large AAA on ultrasound. ICU was also consulted who recommended starting an Esmolol drip to decrease her blood pressure while awaiting their official consult at bedside. Throughout her course in the ED, she was given IV fluids, anti-hypertensives, and multiple medications for her abdominal pain. An A-line was placed to further track her blood pressures. She was stable throughout her entire ED stay and was brought up to the CCU for further management of hypertensive emergency and her AAA.
Following her admission, CTA confirmed a large infrarenal abdominal aortic aneurysm measuring up to 8 cm along with a left common iliac artery aneurysm measuring 2.3 cm. No rupture was found. She was taken to the OR for an open repair and is recovering appropriately.
References:
- https://www.mayoclinic.org/diseases-conditions/abdominal-aortic-aneurysm/diagnosis-treatment/drc-20350693
- https://www.pocus101.com/aorta-ultrasound-made-easy-step-by-step-guide/
- https://coreem.net/core/abdominal-aortic-ultrasound/
- https://aliemcards.com/cards/aorta-ultrasound/
- https://ultrasound.guide/62/abdominal-aorta-transverse-plane
- https://www.acep.org/sonoguide/basic/aorta/
- https://radiologykey.com/abdominal-aortic-aneurysm-ultrasound/
- https://www.lumen.luc.edu/lumen/meded/vc/point_of_care_ultrasound_vc/2018-2019%20labs/shbaortaandivchandout11_2_18.pdf
- https://www.uspreventiveservicestaskforce.org/uspstf/recommendation/abdominal-aortic-aneurysm-screening
