This article was co-posted to REBEL EM emergency medicine blog [Link is here]
Background: Have you considered age when determining whether a resuscitative thoracotomy (RT) is indicated? You’re not alone; over 1/3 of trauma surgeons surveyed consider age before performing a RT (Dennis 2016).
Dr. E. Baue first described RT after cardiac trauma in the 1960s. Many organizations have published guidelines on the procedure and qualifications but none have used age specifically as a decision point. (American College of Surgeons, EAST Trauma Society). Studies have previously attempted to answer this question regarding age as a qualifier for RT. However, most were single-center experiences with different and evolving resuscitation strategies. A recent study used the National Trauma Data Bank found a 100% mortality for patients older than 57 years of age (Gil et al. 2018). Due to the limitations of the available data, further studies are needed looking at age as a predictor for bad outcomes after RT.
Article: Levin J et al. Age Does not Predict Failure to Rescue Following Resuscitative Thoracotomy in Penetrating Trauma. Journal of Emergency Medicine 2021. PMID 33618932
Clinical Question: Does age affect the rate of failure of rescue after resuscitative thoracotomy?
Definitions:
RT is defined as any thoracotomy performed in the ED in patients who:
- Sustained penetrating or blunt mechanism of injury
- In refractory shock
- OR pulseless with cardiopulmonary resuscitation time <15min for penetrating injury
- OR <5min for blunt injury
Population: Patients > 18 years of age who had a RT in the ED following penetrating trauma.
- Patients were identified based on ICD-9/ICD-10 codes.
- Patients were only included if they had a thoracotomy within 15 minutes of arrival, which was designated to assure the RT was being done in the ED.
Outcomes:
- Primary: Failure to rescue (defined as death in the ED despite RT)
- Secondary: Mortality after admission from successful RT
Design:
- Retrospective Analysis
- Data from Trauma Quality Improvement Program (TQIP)
- TQIP is a multi-institutional database assembled by the American College of Surgeons to identify areas of improvement in the dare of trauma patients
Excluded:
- RT in blunt trauma due to negligible survival
- Anyone who underwent RT >15 mins from hospital arrival time to procedure time
- Patients who did not have a pulse on arrival to the ED
Primary Results
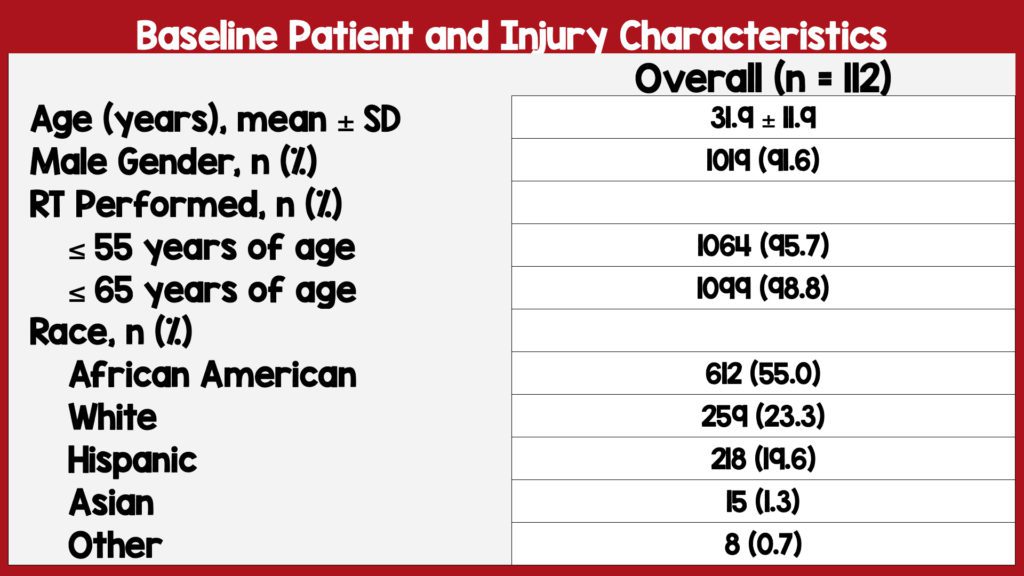
- Identified 1463 who underwent RT in over 850 hospitals
- 1,112 (75%) sustained penetrating injuries
- 96% of RTs were performed in patients ≤55 years of age
- 98% of RTs were performed in patients ≤65 years of age
- 63.6% of patients had multiple injury sites
- The mean age was 31.9 (SD 11.9) with 91.6% of patients being male.
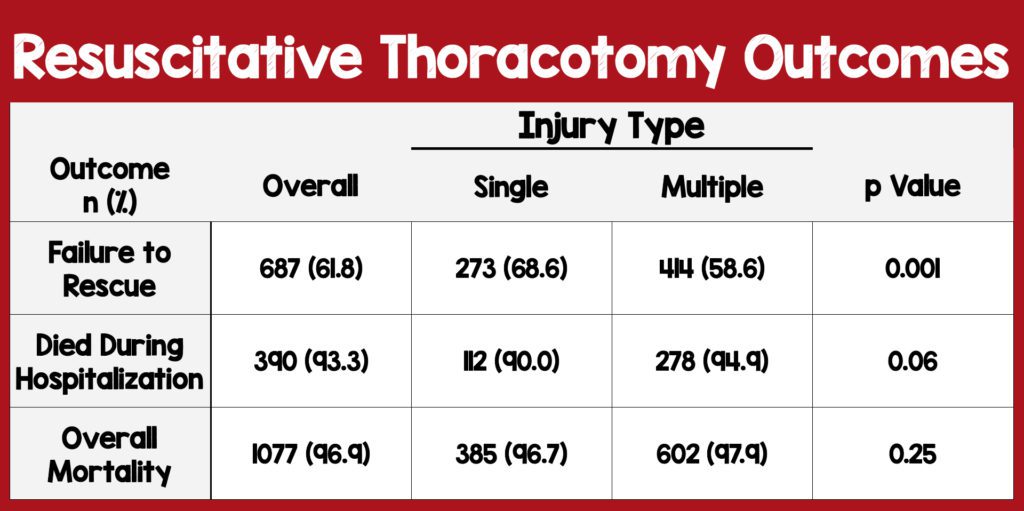
- Failure to rescue was 61.8% (694 died in ED)
- Likelihood of failure to rescue after RT was not significantly associated with age (p=0.44)
- Of those aged ≥55, there were 48RTs performed and a failure to rescue of 32 (66.7%), which was similar to the rate in those <55 (61.7%) p=0.48.
- Of those age ≥65, there were 13RTs performed and a failure to rescue of 8 (61.5%) which was also similar to the rate in those <65 (61.9%) p=0.71.
- Among those who survived to admission (418), 93.3% had in-hospital mortality, yielding a total mortality of 96.9%. Of the patients who were admitted after RT, mortality was not significantly associated with age (p=0.60).
- Univariate analysis showed no association between injury site and mortality across the various age groups.
- Performed 2 multivariate analyses to examine adjusted interaction between mortality and age.
- One adjusted for Injury Severity Score (ISS) and found that age was not an independent predictor for mortality across age groups.
- Second co-adjusted for a multiplicity of injury as well as injury severity and similarly showed that age was not a significant predictor of death (However, in the 60 and 70-year-old age groups, the mortality event rate was too low for proper analysis.)
Strengths:
- Large multicenter data
- Asks a clinically important, patient-centered question
- Broad population without many exclusions
- Multiple analyses were performed to evaluate mortality across age groups including the site of injury and ISS
Limitations:
- TQIP data is not a random sample
- Retrospective study (constraints in its generalizability)
- A smaller sample within older age groups creates a selection bias
- Due to the small sample size of this study investigators could not rule out small mortality benefits
- Used mortality as an outcome yet surviving with a significant disability is a clinically meaningful outcome as well.
- We are unaware of the number of patients who were eligible for RT but didn’t get an RT also leading to selection bias
Discussion
- The study brings awareness to the concept of physiological age not always being equal to chronological age (i.e. Some patients may be older but have minimal medical issues and a good functional status)
- Patients requiring resuscitative thoracotomies present emergently and physicians are typically blinded to pre-existing patient comorbidities and functional status (physiological age). Physicians are forced to decide to perform a RT after making assumptions on the probability of survival from injury mechanism, injury severity, injury location, presenting vital signs, and possibly age.
- This analysis shows that within all age groups there is documented survival, although low, which is distinct from previously published studies on this topic
- The study investigators included 1464 patients who got an RT without mention of the total number of patients with traumatic arrest who were eligible for RT but did not receive it.
- Interestingly, patients with a single injury had a higher failure to rescue rate than patients with multiple injuries (68.6% vs 58.6%) but an overall similar mortality (90.0% vs 94.9%)
- Over a 5 year period, only 48 RTs were performed on patients ≥55 years of age indicates the potential selection bias of this study
- Older patients who receive an RT may have been cherry-picked from a cohort of older patients who were perceived to do better, which can bias results in favor of the older group.
- If trauma surgeons believe RT would be futile because of advanced age and comorbidities they won’t perform an RT
- Trauma surgeons may be more likely to do a RT on an 18-year-old even if they think there’s no chance of a good outcome.
- Resulting in a perceived worse outcome for the younger group, again biasing the results in favor of the older group.
- Would be enlightening to see the data on patients who were eligible for RT but didn’t get an RT.
Authors Conclusions: “Age does not appear to be an independent predictor of failure to rescue or survival after RT in penetrating trauma and should not be the sole determinant determining candidacy for RT. The decision to perform a RT in penetrating trauma should incorporate multiple indicators of salvageability, including patient physiology, injury pattern, and markers of frailty. Further studies are needed to identify such metrics.”
Our Conclusions: In this study, older age was not associated with worse outcomes of RT. However, the inherent selection bias renders the data of limited utility to make any conclusions about age and failure to rescue in penetrating trauma patients.
Clinical Bottom Line:
Age alone should not be used as a hard stop on penetrating trauma victims requiring RT. Unfortunately, this study does not help guide us in clinical practice and future work should seek to gather all patients who would have been eligible for RT to give us information that gets us closer to the truth.
Post By:

Sergio Camba, MD
PGY-1, Emergency Medicine Resident
Saint Joseph’s Regional Medical Center, Paterson New Jersey
Twitter: @Sergio_Camba
[Hi-Res Photo]
Joe Bove, DO
Assistant Professor, Emergency Medicine
Saint Joseph’s Regional Medical Center, Paterson New Jersey
Email: [email protected]
[Hi-Res Photo]
Steven Hochman, MD FACEP
Associate Professor, Emergency Medicine
Saint Joseph’s Regional Medical Center, Paterson New Jersey
Twitter: @hochmast
Read More
Bibliography
- Boyd M, Vanek VW, Bourguet CC. Emergency room resuscitative thoracotomy: when is it indicated? J Trauma. 1992 Nov;33(5):714-21. PMID: 1464921
- Hunt PA, Greaves I, Owens WA. Emergency thoracotomy in thoracic trauma-a review. Injury. 2006 Jan;37(1):1-19. doi: 10.1016/j.injury.2005.02.014. Epub 2005 Apr 20. PMID: 16410079
- Pust GD, Namias N. Resuscitative thoracotomy. Int J Surg. 2016 Sep;33(Pt B):202-208. doi: 10.1016/j.ijsu.2016.04.006. Epub 2016 Apr 14. PMID: 27102328
- Segalini E, Di Donato L, Birindelli A, Piccinini A, Casati A, Coniglio C, Di Saverio S, Tugnoli G; Bologna Trauma Team collaborative group. Outcomes and indications for emergency thoracotomy after adoption of a more liberal policy in a western European level 1 trauma centre: 8-year experience. Updates Surg. 2019 Mar;71(1):121-127. doi: 10.1007/s13304-018-0607-4. Epub 2018 Dec 26. PMID: 30588565
Post Peer Reviewed By: Anand Swaminathan, MD (Twitter: @EMSwami) and Salim R. Rezaie, MD (Twitter: @srrezaie), Marco Propersi, DO (Twitter: @marco_propersi)