CC: “Post Surgical Pain” ; Abdominal pain
HPI: 8 year old Male with PMH of Sickle Cell Disease (HbSC), Post-opt Day 10 for laparoscopic splenectomy for recurrent sequestration crises presents to the Emergency Department (ED) complaining of abdominal pain x 2 days. The pain is described as diffuse and worse in the RUQ. Denies exacerbating or relieving factors. Pain is associated with constipation; last Bowel movement was 7 days prior. Mother states he did have one small BM shortly after surgery. He is tolerating PO without difficulty and does report flatus. She has been giving him Oxycodone 2mg every 6 hours for pain with minimal relief. Upon review of systems, patient reports feeling hot for the past 2 days but without a recorded temperature at home. Additionally, patient complained of a non-productive cough for 2 days and has been “breathing fast” for the same duration of time.
Physical Exam:
BP 112/74 HR 129 RR 24 SpO2 93% on RA Temp 99.9F 26.3 kg
Constitutional: Well developed, well-nourished child who is awake, alert and in moderate distress due to pain and feeling hot; making tears
HEENT: NCAT, pupils PERRLA, neck supple
Respiratory: CTA B/L, no wheezing, rales or rhonchi
Chest/Axilla: Normal symmetrical motion, no tenderness
Cardiac: +S1/S2, RRR, no MRG,
Abdomen: Scars noted over splenectomy site which are clean dry and intact, healing well without discharge; Diminished Bowel Sounds in all quadrants; soft, non-distended with mild tenderness in all 4 quadrants. No rebound or guarding.
Neuro exam: AAO x 3. No deficits
Extremities: no edema, no tenderness or swelling
Pertinent Labs:
CBC: 42.1
HBG: 12.5
HCT: 36.9
Platelets: 721
Seg: 79
Lymphs: 9
Mono: 12
Reticulocyte count: reported as normal
Pertinent Imaging and other tests:
Working Diagnosis:
Generalized abdominal pains
Elevated WBC
Abscess of spleen
ED/Hospital course:
Surgery was consulted in the ED and they believed the pain was not related to the surgery. Abdominal U/S performed at their request showed “s/p splenectomy with gallbladder sludge.” Patient had moderate improvement in his pain after Toradol 15mg IV and Morphine 2mg IV were given in the ED. Patient also received Rocephin 75mg/kg and NS 500mL IV Fluid bolus for presumed infection with the leukocytosis of 42.1.
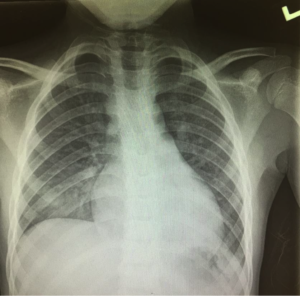
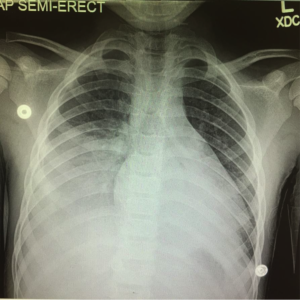
The patient was admitted to Pediatric Step down for further evaluation and management. Overnight, he remained comfortable with stable vital signs, afebrile and saturating 94-96% on 2L NC. On Hospital day #1, patient became febrile to 103F and continued to deny chest pain, SOB or difficulty breathing. The cough remained unchanged since admission. A repeat Chest X-Ray was obtained and the patient was diagnosed with Acute Chest Syndrome and received exchange transfusion the same day (Refer to Image below) Additionally, he received Ceftriaxone, Azithromycin, Nitric oxide and IVF at ¾ maintenance ate throughout hospitalization. On Hospital Day #4 he was discharged home.
Pearls:
Acute Chest Syndrome
- It is the leading cause of death in patients with SCD in the United States
- Most often occurs as a single episode, but patients may have multiple attacks resulting in chronic lung disease
- Multiple Etiologies
- Pulmonary infections
- Iatrogenic cause including aggressive hydration for sickle cell painful crisis ——à causing Pulmonary Edema
- Opioid use —–à Decreased inspiratory effort——à Atelectasis
- New infiltrate identified on Chest X-Ray with at least one of the following: Fever, cough, wheezing, tachypnea, chest pain, hypoxemia.
- Radiographic changes often lag behind clinical features so initially the Chest X-Ray may actually be normal (as in our case)
- Treatment
- Supportive: Early Supplemental Oxygen, analgesics and IV Hydration up to 1.5x maintenance rate
- Antibiotic irrespective of cultures
- Transfusion is believed to be lifesaving; recommendations based on empirical observations and not on firm evidence
- Exchange transfusion seems to be more advantageous, especially in patients with a hemoglobin of > 9.0
- It decreases the concentration of sickled hemoglobin with little iron gain
- Inhaled Nitrous Oxide is beneficial
- Due to its vasodilatory effects –à improved ventilation/perfusion in damaged lung tissue
- Reduced RBC and leukocyte adhesion to endothelial cells, therefore affecting disease progression
- Hydroxyurea reduces occurrence of acute chest syndrome
Case Presented by Greg Cassidy, MD
References:
- Stapczynski, J. S., & Tintinalli, J. E. (2016). Tintinalli’s emergency medicine: A comprehensive study guide (8th ed.). New York, N.Y.: McGraw-Hill Education LLC..
