CC: Nausea and vomiting and “ I think my sugar is low”
HPI: 36-year-old Female with PMH of Diabetes presents to the Emergency Department complaining of multiple episodes of non-bloody, non-bilious vomiting for the past 5 days. Associated symptoms include chills and a mild sore throat. Denies fever, HA, neck pain, chest pain, SOB, abdominal pain, diarrhea or bloody stools. Denies dysuria, hematuria or urinary frequency or urgency. Denies recent travels or sick contacts. LMP: Currently menstruating
PMH: Diabetes
PSH: C-Section
Meds: None
Allergies: NKDA
Social: Admits to smoking 2 cigarettes per day for the past 10 years. Smokes marijuana daily. Denies alcohol use
Physical Exam :
BP 171/82 HR 82 RR 20 SpO2 100% on RA Temp 97.8F 108.86 kg
Constitutional: Alert, wake, and in no acute distress. Obese
HEENT: NCAT, pupils PERRLA, neck is supple. Oral mucosa is pink, dry and intact. No lesions. Normal conjuctiva
Respiratory: CTA B/L, no rales, rhonchi, no stridor or wheezing
Cardiac: +S1/S2, regular rate and rhythm, no murmur, rubs or gallop
Abdomen: Soft, with mild tenderness in epigastric area. No rebound or guarding. Normal BS
Neuro: AAO x 3. No focal deficits, moving all four extremities. Steady gate without difficulty.
MSK/Extremities: no edema, tenderness or swelling.
Skin: Moderate ecchymosis overlying RUQ and RUE. Normal moisture. No rash or lesions noted
Pertinent Labs:
WBC: 8.4 HGB: 9.3 HCT: 26.8 Platelet: 9L
Na: 136 K: 3.4 Cl: 104 Co2: 26 BUN: 16 Cr: 0.95 Glucose: 109
PT: 14.4 PTT: 28.7 INR: 1.1
Calcium 8.8 Total Bilirubin: 2.8 Alk Phos: 56 AST: 21 ALT: 12
Lipase: 60
UCG: negative
Urinalysis: Large Blood with negative Nitrites and Leukocyte Esterase without ketones. UA Protein: 100
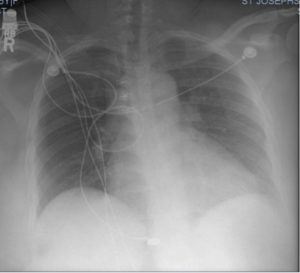
Pertinent Images and other tests: Chest X ray: Borderline heart size. NO active disease
Upper Abdominal U/S: Normal Liver and spleen. The spleen measured 10.9 cm in greatest dimension and was homogeneous in echotexture. No focal splenic lesion identified. The liver measured 16.5 cm and appeared normal.

EKG:

Working Diagnosis:
Thrombotic Thrombocytopenia Purpura (TTP)
Idiopathic Thrombocytopenic Purpura (ITP)
Hemolytic Uremic Syndrome (HUS)
Anemia due to blood loss
Infection/Sepsis
ED Course: On further questioning, patient states she has been menstruating for 3 weeks now and bleeding is heavier as compared to the previous cycle. In the ED, patient was given NS 0.9% 1000mL IV bolus once, Zofran 4 mg IV once, Reglan 10mg IV once. Type and screen and blood cultures were also sent and patient was admitted to the Medical ICU for thrombocytopenia and anemia.
Hospital Course:
In the Medical ICU, further lab results demonstrated elevated the following:
LDH: 699 Fibrinogen: 410 Haptoglobin: < 10 Troponin 0.44
Blood Cultures: No Growth
Urine Toxicology: Positive for cannabinoids
Hepatitis C antibody: < 0.1
HIV Ag/Ab: Non reactive
In the ICU, patient was given a 125mg bolus of IV Solu-Medrol and then started on 60mg IV every 8 hours. She was transfused 1 Unit of platelet with no response, as the following day, platelets actually dropped to 5.Hematology/Oncology was also consulted. They stated that the occasional schistocytes seen on blood smear with low Haptoglobin levels and elevated reticulocyte count and LDH was suggestive of microangiopathic hemolytic anemia, making TTP a more likely diagnosis. Heme/Onc recommended against any further platelet transfusion and ADAMS 13 levels were sent. On hospital day #3, patient’s LDH levels had increased to 1586 and Troponin was elevated to 1.2 with symptoms of dyspnea. Patient also had worsening anemia as hemoglobin dropped to 7.0, and platelets remained at 9. The same day, Surgery was consulted and patient was transfused 2 Units of PRBs and 2 Units of FFP in preparation for Shiley Catheter insertion for plasmapheresis. Cardiology was also consulted for the elevated troponin, which they attributed to ongoing demand ischemia without any evidence of ACS. Unfortunately, the following night at 1:25 AM and before a Shiley was ever placed, the patient became minimally responsive and Saturating at 90% on RA. Immediately, she became bradycardic and lost pulses. CPR was initiated as patient was simultaneously intubated. Total duration of CPR was 60 minutes. The patient received Epinephrine x 20, Amiodarone 300 mg x 1 and Insulin with 1 amp of D50W, Calcium chloride and Sodium Bicarbonate for Potassium of 6.1 on ABG. Sadly, the patient was pronounced at 2:25AM.
PEARLS : Thrombotic Thrombocytopenic Purpura (TTP)
PENTAD = ‘FAT RN”
- Fever (50%)
- Uncommon if they present early in the disease
- High fever and chills suggest sepsis, so look for a source of infection.
- Thrombocytopenia
- MAJOR diagnostic criterion
- Mean platelet of 25, 000 but they reach 5000.
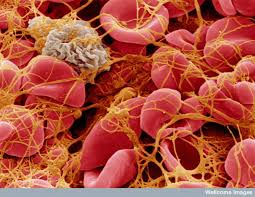
- Microangiopathic Hemolytic Anemia
- MAJOR diagnostic criterion
- Non-immune hemolysis with schistocytes
- Results in elevated LDH, Low haptoglobin and high indirect bilirubin
- Severely elevated LDH has been associated with MI, arrhythmias, shock and heart failure.
- Renal Failure
- Due to renal thrombotic microangiopathy
- Urinalysis will show mild proteinuria +/- hematuria
- Acute Rena insufficiency may be present and may require dialysis.
- Neurological Symptoms: (Seizure, AMS, HA, coma, hemiplegia, aphasia, etc.)
- Focal Deficits less prevalent
- Occurs in 25-60% of patients
- Symptoms are usually transient and subtle, so you must ask the patient about prior symptoms!
*** KEEP in mind; all features of the PENTAD do NOT to be present at the same time for diagnosis to be made.
Risk Factors
- Obesity
- African American race
- Female
- Ages 30-50 years
- HIV/AIDS
- Rheumatologic/autoimmune disease history
Clinical Presentation
- Fatigue, tachycardia, pallor, SOB or chest pain
- Abdominal pain, back pain, Nausea, vomiting or diarrhea
- New Onset jaundice and dark colored urine
Physical Exam
- Diffuse, non-palpable petechial/purpuric rash.

Etiology
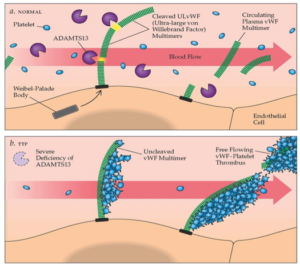
- ADAMTS-13 protease enzyme deficiency
- 60% of cases
- Enzyme cleaves von Willebrand factor (vWF) multimers. Without it, excessive platelet aggregation, thrombocytopenia and thrombosis occurs
- Idiopathic or Secondary Causes
- 40% of cases
- (i.e. HIV, malignancy, Infection, Pregnancy, pancreatitis, autoimmune disease, pancreatitis and medications such s Acyclovir, Quinine, Oxymorphoine, Plavix and Tacrolimus)
- Diagnosis/Lab findings
- NORMAL PT, PTT and Fibrinogen levels (Unlike in DIC)
- Thrombocytopenia
- Anemia and elevated indirect bilirubin
- A peripheral smear is important for diagnosis, as 100% of patients will have schistocytes present during the course of the disease
- ADAMTS-13 activity < 10% (normal activity is > 50%)
*** Remember that TTP is a clinical diagnosis. Do NOT delay treatment!
- Differential Diagnosis
- Other Causes of Microangiopathic Hemolytic Anemia (MAHA)
- DIC, HUS, HELLP Syndrome, Malignant Hypertension, Heparin induced thrombocytopenia, Paroxysmal Nocturnal Hemoglobinuria, etc.
- ITP
- Sepsis
- SLE
- Viral infections (HIV, mumps, varicella, EBVS)
- Other Causes of Microangiopathic Hemolytic Anemia (MAHA)
- Management
- Consult Hematology!
- AVOID Platelet Transfusion if possible!
- It can lead to renal failure, higher rates of arterial thrombosis and death
- Should be AVOIDED EXCEPT in life-threatening bleeding or ICH
- Plasma Exchange (Plasmapheresis) is First Line treatment!
- Replaces defective or insufficient ADAMTS-13 and clears vWF multimers
- LDH can be used to evaluate for treatment response
- FFP Transfusion
- Contains ADAMTS-13
- Can be helpful if delay in plasmapheresis
- Transfusion of RBCs (indicated ONLY in severe bleeding with a delay in plasma exchange)
- Glucocorticoids
- Adjunct Treatment and do not replace plasmapheresis
- 1mg/kg Prednisone PO or Solu-Medrol 125mg IV
- IVIG
- Not first line but may be used in those who fail plasmapheresis
- Splenectomy
- Last line therapy after stabilization
- Inhibitor antibody is made in the spleen
Suspect TTP in any patient with MAHA and thrombocytopenia!
Case presented by Dr. Yenisleidy Paez Perez, DO