
CC: Can’t see for 2 months
HPI: 10 year old male with no significant past medical history presents to the Emergency Dept. complaining of painless vision loss in the right eye for 2-3 months. Patient states he has been having difficulty seeing out of his right eye for 2 months despite changing positions in class, taking on and off his glasses and using eye drops. Vision loss has become progressively worse and now he can only distinguish whether lights are on or off. Mother states she did not do anything about this problem because she thought he was kidding and she didn’t’ have money or health insurance to seek medical attention. Patient has been wearing Bifocals for myopia since the age of 6, with corrective vision lenses at age 5. Denies associated trauma. Patient moved to the U.S from Nigeria 5 years ago. He lives with his mother and sister. Vaccines are up to date.
PMH/Birth History: NSVD at 39 weeks, 1 day. Birth took place in Nigeria and mother denies any infection during or after pregnancy. Following birth, patient did not have any complications such as pneumonia, eye infections or rashes.
Social History: Denies drug abuse. Denies exposure to chemicals. Denies contact with dirt, dogs or pigs. Patient did not live on a farm. As per mother, there was no domestic abuse in the family
PHYSICAL EXAM
Vitals within normal Limits
General: In no acute distress, appears stated age.
Head: Atraumatic, normocephalic. No deformities.
Eye: Right (OD): pupil non-reactive and remains white in color and approximately 2mm. Afferent reflex is present CN II; efferent reflex is absent. There is a complete visual field defect on the right side. Visual Acuity: Can only distinguish between light and dark. Unable to count fingers at any distance or visual objects even in motion. On Fundoscopic exam, the fundus is gray/dull, with no retina visualized. ALL CONSISTENT WITH LEUKOCORIA
Respiratory: Lungs CTA bilaterally.
Cardiac: +S1/S2, no MRG, regular rate and rhythm
Abdomen: soft NT ND
Neuro exam: CN III –XII intact. No motor, sensory, vibratory, temperature or pain deficits. Gait is steady and normal, without any difficulty. Cerebellar function intact, no dysmetria bilaterally.
Extremities: Full ROM in all extremities. 5/5 strength in all extremities
Skin: No edema, rashes, lacerations, or abrasions. Skin is warm, pink, moist and intact.
LABS
CBC: Unremarkable with WBC: 7.1 Hemoglobin: 13.5 Platelets 211.
CMP: WNL CRP and ESR = WNL
Tonometry: IOP approx. 17-18 x 3 times
Wood lamp: No corneal abrasion, dendritic ulcers, lesions or depositions OU
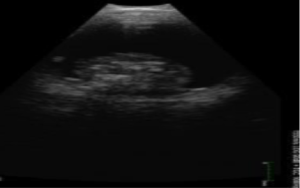
Bedside U/S: Completed within 10 minutes of arrival ( Only Right eye is shown)


Working Differential Diagnosis:
- Retinoblastoma
- Intraocular Mass
- Cataract
- Syphilis
- Parasitic infiltrate
- Posterior Infarct
CT Max/Facial w/o Contrast to rule out intracranial pathologies: Negative for masses; positive for homologous material in the right lobe. MRI was recommended for further evaluation


ED/Hospital course: Ophthalmologist on call was consulted, and said there was nothing more to do. Unfortunately because his vision loss was > 2 months, no life saving surgery was imminent as the retina was already detached causing ischemia to the rods and cones within it. Patient was to follow up in ophthalmology clinic the following day. Patient’s Pediatrician was also contacted and he referred the patient to a Pediatric Ophthalmic specialist in University Hospital, with a scheduled appointment within the same week. Approximately one week ago, patient underwent surgery and the leading diagnosis was Toxocariasis as per MRI. Biopsy results to follow. As per mother, the patient is still without vision in his right eye.
| LEUKOCORIA, UNILATERAL, 10 YO MALE DIFFERENTIALS
Coats disease— is an exudative retinal vascular disorder characterized by retinal telangiectasias and subretinal exudation leading to serous retinal detachment. Presenting complaints include decreased visual acuity, strabismus, or leukocoria. The leukocoria in Coats disease is generally more yellow than white due to the presence of subretinal lipid. Coats disease is almost always unilateral and the vast majority of cases occur in boys. The majority of cases presenting with leukocoria are diagnosed between five and nine years of age, which is older than the majority of retinoblastoma patients. Clinical examination: subretinal lipid and abnormal telangiectatic vessels US: demonstrates complete retinal detachment with massive subretinal lipid. Intraocular calcification is almost never present in Coats disease, another feature that helps to distinguish it from retinoblastoma.
|
| Toxocariasis — Toxocariasis, or visceral larva migrans, is an infection caused by the dog ascarid Toxocara canis or, less commonly, the cat ascarid Toxocara catis. There may be a history of living in an underdeveloped country, and exposure to dirt or undomesticated dogs. It occurs most commonly in children one to five years of age. Common presenting signs of toxocariasis are strabismus and poor vision. The ocular lesion is caused by the inflammatory response to the second-stage larva, which may localize in the one eye or both eyes
|
Retinopathy of prematurity (ROP) — developmental vascular proliferative disorder that occurs in the incompletely vascularized retina of preterm infants and can lead to retinal detachment and permanent blindness. The most important risk factor for developing ROP is prematurity. There needs to be a history of prematurity, and/or mother mentions patient was on O2 for awhile.
Vitreous hemorrhage — Vitreous hemorrhage causes leukocoria when there is extensive organization of the blood into a clot before degradation. With time, the reddish hue of the blood is lost and the hemorrhage transforms into “whitish debris.” Etiology includes advanced ROP, trauma (MOST common), leukemia or hemorrhagic disease of newborn
Retinablastoma– Retinoblastoma is the most common primary intraocular malignancy of childhood and accounts for 10 to 15 percent of cancers that occur within the first year of life. Retinoblastoma typically presents as leukocoria in a child under the age of two years. Untreated retinoblastoma is a deadly disease; however, with advances in treatment, survival in the contemporary era is >95 percent. Most common age group is birth- 2 years. Very uncommon in children over the age of 5, although 1-2 case reports have occurred in 18 year old males

Pearls & Takeaways:
- Leukocoria Requires further investigation – On exam, History and Diagnostic
- The use of tonometry, fundoscopy and ocular ultrasound are an easy, noninvasive way to add to your ophthalmic exam. Slit-lamp exam could have been considered here
- Ocular ultrasound is really cool and fun!
- Advocate for your patients! Make sure they have proper follow up with a specialist
- If any abuse or neglect is suspected, be sure to turn on “Sherlock Holmes” senses and investigate.
Case presented by Dr. Sarah Bolan
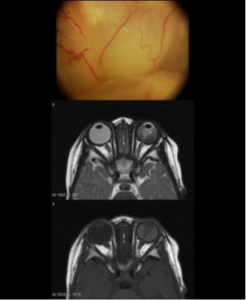 The retinal photograph depicts bullous retinal detachment in the Left eye of a 1-year-old child with Coat’s disease simulating retinoblastoma. The magnetic resonance images confirm the diagnosis of retinal detachment and exclude retinoblastoma because of the absence of intraocular mass.
The retinal photograph depicts bullous retinal detachment in the Left eye of a 1-year-old child with Coat’s disease simulating retinoblastoma. The magnetic resonance images confirm the diagnosis of retinal detachment and exclude retinoblastoma because of the absence of intraocular mass.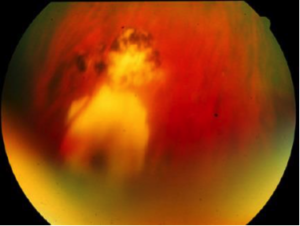 Chorioretinitis characteristic of toxoplasmosis. A pigmented scar is seen with an adjacent area of active chorioretinitis. The diagnosis of toxoplasmosis is based primarily on the appearance of the chorioretinal lesion rather than serologic studies. Courtesy of James T Rosenbaum, MD.
Chorioretinitis characteristic of toxoplasmosis. A pigmented scar is seen with an adjacent area of active chorioretinitis. The diagnosis of toxoplasmosis is based primarily on the appearance of the chorioretinal lesion rather than serologic studies. Courtesy of James T Rosenbaum, MD.