Pediatric Pearls – September 2018
INFLUENZA
By: Hima Khamar M.D., PGY3
During flu season we see many patients with flu-like illness. Which of these patients should be tested and treated? Which of these patients require no testing, just supportive treatment?
SIGNS & SYMPTOMS:
Fever > 100.4°F (or 38°C), Chills, Cough, Body aches, Headache, Sometimes diarrhea and vomiting
WARNING SIGNS:
Respiratory distress
Cyanosis, hypoxia
Decreased PO intake
Signs of dehydrations: no tears when crying, significantly fewer wet diapers than normal, decreased capillary refill
Lethargic
If patient has warning signs, THEN ADMIT!
Test for Flu A/B and RSV -> if positive for flu A/B, then treat
STABLE PATIENTS WHO SHOULD BE TESTED:
(1) Less than 12 months with the following chronic conditions:
-Pulmonary (e.g., Asthma), cardiac, renal, hepatic, hematologic, metabolic, neurologic
-Immunosuppressed, or household contact who is immunosuppressed
-Long term ASA therapy
-Morbid obesity
-Resident of chronic care facility
(2) 12-24 months who are moderately ill, but have no warning signs
(3) Consider testing in those patients who have siblings <6 months or high-risk siblings with chronic conditions
STABLE PATIENTS WHO SHOULDN’T BE TESTED:
-Previously healthy children > 24 months old
TREATMENT:
If tested and positive, then TREAT
Oseltamivir (5 days)
-If younger than 1 yr old: 3 mg/kg/dose twice daily
-If 1 yr or older, dose varies by child’s weight:
<15 kg, the dose is 30 mg twice a day
-15 to 23 kg, the dose is 45 mg twice a day
-23 to 40 kg, the dose is 60 mg twice a day
>40 kg, the dose is 75 mg twice a day
AMERICAN ACADEMY OF PEDIATRICS (AAP) RECOMMENDATIONS
FOR FLU VACCINE 2018-2019
“This season, the AAP recommends that pediatricians offer the injectable form of the vaccine to all children 6 months and older as soon as it becomes available, preferably by the end of October.”
“The AAP recommends the injectable flu vaccine (trivalent or quadrivalent) as the primary choice for children because it has provided the most consistent protection against all strains of the flu virus in recent years.”
“Effectiveness of a live attenuated influenza vaccine against influenza A(H1N1) was inferior during past influenza seasons and is unknown for this upcoming season.”
CROUP (LARYNGOTRACHEOBRONCHITIS)
By: Hima Khamar M.D., PGY3
Background:
-Viral illness
-Most common in late fall to early winter
-Results in inflammation and swelling of the upper airway
Causes:
-Parainfluenza (most common)
-RSV
-Influenza A and B
-Other respiratory viruses
Signs and symptoms:
-Sudden onset of barky cough
-Hoarse voice
–INSPIRATORY Stridor
-Mild to moderate respiratory distress
– +/- Fever
-May be preceded by mild URI symptoms
-Symptoms tend to be worse at night
-Usually resolve within 48 hours
| HISTORY | PHYSICAL |
| 1. Duration of: stridor, cough, hoarse voice 2. Fluctuation of symptoms over the course of the day (worse at night or when waking up from nap) 3. Hydration 4. History of sudden onset of choking (concern for foreign body) 5. Exposure to allergen, heat, or chemicals 6. PMH: intubation, tracheostomy, airway/esophageal surgery, prior croup |
1. Vital signs, pulse oximetry 2. Overall appearance 3. Mental status 4. Respiratory status: retractions, barky cough 5. Hydration status 6. Symmetry on respiratory exam 7. Lack of drooling |
DIAGNOSTICS
-No need to obtain chest x-ray
-No need to send viral panel
–THIS IS A CLINICAL DIAGNOSIS!
| SYMPTOMS | |
| MILD | MODERATE/SEVERE |
| – Barky cough, hoarse voice – No stridor at rest – Mild coarse stridor – Stridor only during agitation/activity – No or mild WOB |
– Anxiety, mental status changes – Stridor at rest – Moderate, severe work of breathing – retractions, tachypnea, difficulty talking or feeding – Hypoxemia |
| TREATMENT | |
| MILD | MODERATE/SEVERE |
| DEXAMETHASONE (0.3 mg/kg, MAX 8 mg) – No difference in IM or PO – No indication to give repeat doses |
DEXAMETHASONE (0.6 mg/kg, MAX 12 mg)
RACEMIC EPINEPHRINE (2.25% sln, 0.5 mL in 3 mL NS) Observe for 2 hours after administration of racemic epinephrine |
DISCHARGE CRITERIA
-No or minimal coarse stridor at rest (expect stridor with activity)
-No or minimal retractions
-Able to tolerate PO feeding
CONSIDER ALTERNATIVE DIAGNOSIS
Main alternative diagnosis to consider is bacterial tracheitis (toxic appearing child with progressive symptoms)
-Age <6 months or >6 years
-Poor response to treatment
-Duration of stridor >4 days or cough > 10 days
-Non-elective intubation in past 6 months
-Prolonged intubation
-Recurrent croup: 2nd episode in 30 days or >3 episodes in last 12 months
-Toxic appearance
-Drooling, difficulty swallowing, severe anxiety
-Asymmetry of respiratory exam
Pediatric Pearl – August 2018
FEBRILE INFANT
By: Hima Khamar, PGY3
The plan for a febrile infant who is <28 days is easy. We know what to do (labs, LP, antibiotics, and admit). But what to do with that 29-56 day old who is well appearing. Do we need to go down the entire pathway? Do we need to LP? Can we discharge some of them home? I hope this month’s pediatric pearl gives you a little more insight into that undifferentiated febrile infant.
Why are we so worried about fever in these infants? It’s because these little guys/gals can’t fight off infection that well. We worry about whether this is just a viral infection or a serious bacterial infection (SBI). Most of the time it is just a viral infection, but missing an SBI can lead to catastrophic consequences for the patient. Additionally, these patients can appear well, but be harboring an SBI that can lead to decompensation if not treated early.
Consider this pathway for infants <56 days with rectal/axillary temp >38°C (100.4°F) in ED, at home, or PMD office
HISTORY:
Height, duration of fever
Tylenol use, method of temperature measurement
Oral intake / urine output in past 24 hours
Presence of vomiting/diarrhea, loss in past 24 hours
Change in behavior
URI symptoms
Rash, ill contacts, recent immunizations or antibiotics
PHYSICAL:
Vital signs – tachypnea, tachycardia, hypoxia, hypotension, febrile (how high)
Weight
General appearance – sick or not sick (lethargy, tone, irritability, not consolable)
Fontanelles
Respiratory exam – wheezing, rales, rhonchi
Cardiac exam – murmurs
Abdominal exam – masses, organomegaly
GU exam – lesions
Skin exam – rashes
Neuro – deficits, seizures
PMH:
- Birth history
- Pregnancy, delivery, prematurity, birth weight
- NICU, newborn nursery course
- Vaccination history
- Infectious risk factors
- Maternal fever or history of infection:
- Group B strep, maternal treatment
- Gonorrhea, chlamydia, or syphilis
- HSV, lesions during perinatal period
- HIV
Newborn screen results – normal or abnormal
DIAGNOSTICS:
- IV access, O2 if needed, monitor
- CBC, blood culture x 1 (only need 1)
- BS (if needed)
- UA and Urine culture
- LP (if needed) with CSF studies (Culture, Gram stain, glucose, protein, cell count with differential, viral studies, any other specific studies based on history and risk factors)
- CXR (if needed, depending on sxs)
- Stool cultures (if having diarrhea)
- RSV/FLU depending on season and sxs
TREATMENT:
- IVF 20cc/kg followed by maintenance fluids
- Antipyretics – Tylenol (no Motrin until 6 months of age)
- Antimicrobial Therapy:
| 0-28 Days | 1. Ampicillin (GBS, enterococcus, listeria)
2. Cefotaxime (strep B, H. flu, E.coli) 3. Acyclovir (HSV) 4. +/- Vancomycin if MRSA is a concern |
| 29-56 Days | 1. Ceftriaxone or cefotaxime
2. +/- Ampicillin depending on what bugs you are targeting 3. +/- Acyclovir again depending on suspicion 4. +/- Vancomycin if MRSA is a concern |
Over the years there have been three main risk stratification tools used: Rochester, Boston, and Philadelphia. Each of these have similarities and some minor differences. Neither has been shown to be better than the other. Below I have outlined the three criteria for your reference.
| ROCHESTER | BOSTON | PHILADELPHIA | |
| Age | <60 days | 28-89 days | 29-56 days |
| Temperature | 38°C | 38°C | 38.2°C |
| History and Physical | Full term. No perinatal complications. No hospitalized longer than mom. No history of chronic or underlying disease. No previous abx use. No ear, soft tissue, joint or bone infection. No previous hospitalization. No treatment for unexplained hyperbilirubinemia. | No recent immunizations, no antibiotics. Full term. Well appearing, normal PE. | Well appearing. No focal infection. |
| CBC | 5000-15000 | <20000 | <15000 |
| Band | <1500 | Bands:neutrophil à <0.2:1 | |
| Urinalysis | <10 WBC/HPF | <10 WBC/HPF or negative for leukocyte esterase | <10 WBC/HPF and few/no bacteria |
| Stool (if indicated) | <5 WBC/HPF | Negative | |
| CSF | <10 WBCs/HPF | <8 WBCs/HPF | |
| CXR | If obtained, negative | No infiltrate | |
| High risk | Admit + IV ABX | Admit + IV ABX | Admit + IV ABX |
| Low risk | Home
No ABX Follow up with pediatrician |
Home
No ABX Follow up with pediatrician |
Home
Empiric antibiotics Follow up with pediatrician |
| Sensitivity | 92% | Not available | 98% |
| Specificity | 50% | 94.6% | 42%% |
| NPV | 98.9% | Not available | 99.7%% |
NEW KID ON THE BLOCK: STEP BY STEP (<90 days)
Fever = >38°C Sensitivity 92.0% ; NPV 99.3%
Abnormal Pediatric Assessment Triangle? Ill appearing? ————> YES———-> HIGH RISK
(pediatric assessment triangle – circulation, work of breathing, appearance)
NO
age < 21 days———–> YES————> HIGH RISK
NO
Leukocytouria——————-> YES————->HIGH RISK
NO
Procalcitonin > 0.5—————-> YES————–> HIGH RISK
NO
CRP > 20 OR ANC> 10000—————–> YES—————> INTERMEDIATE RISK
NO
LOW RISK PATIENT
These are some of the tools we have to help risk stratify the undifferentiated febrile infant. I would use caution in applying these to infants <28 days. I encourage you to read the articles from which these criteria came from.
Pick one and apply it! REMEMBER ALWAYS, YOUR CLINICAL GESTALT ALSO MATTERS!
Pediatric Pearl – July 2018
Brief Resolved Unexplained Event (BRUE)
The Artist Formerly Known as Apparent Life-Threatening Event (ALTE)
By: Kerri Clayton PGY-3
In 2016 The American Academy of Pediatrics (AAP) released clinical practice guidelines on Brief Resolved Unexplained Events (BRUE) in low-risk infants, and at this time changed the name from Apparent Life-Threatening Event (ALTE). This is the first AAP guideline that specifically addresses these events. The new guideline and change in terminology from ALTE are based on a literature review of ALTEs from 1970 through 2014.
Why the change the name?
- More precise
- Has age limits
- It highlights the reassuring qualities of the episode: Brief and Resolved
What is a BRUE?
- An Event lasting <1 minute in an infant <1 year of age that is associated with at least one of the following:
- Central Cyanosisor Pallor
- Discoloration of face, gums and/or trunk.
- NOT acrocyanosis, only peri-oral cyanosis or rubor
- Absent, Decreased,or Irregular breathing
- Central, obstructive or mixed apnea
- NOT periodic breathing or breath holding spell
- Marked change in tonesuch as hypertonia or hypotonia
- Altered level or responsiveness
- It MUST resolve, and the patient must be at baseline, have a reassuring history, physical exam, and vital signs during Emergency department evaluation.
- IMPORTANT: The term BRUE is used only when there is no other likely explanation, meaning that a clinician is unable to explain the cause of the event after an appropriate H&P.
- Examples:
- respiratory symptoms and fever; NOT a BRUE.
- choking or gagging associated with spitting up; NOT a BRUE
History
- Event characteristics
- Preceding illness or injury
- Event description
- location, position, feeding, environment
- choking, gagging
- tone, movement
- mental status
- level of distress
- color change – blue, pallor, red
- breathing ability – apnea, shallow breathing or difficulty breathing
- duration, intervention return to baseline
- Pertinent past
- Prematurity (<32 wks)
- Previous episode/BRUE
- Newborn screening results
- Growth and development
- Breathing problems
- Reflux
- Medications
- Family
- Sudden unexplained death
- Cardiac disease, arrhythmias
- Metabolic/genetic disease
- Social
- Environment, exposures, illness contacts
- Family structure, individuals at home
- Caretakers, stressors
- Consideration for possible child abuse
Physical Exam
- Vital signs – Temp, HR, RR, BP, O2 sat
- Growth – weight, head circumference
- General appearance – craniofacial abnormalities, age-appopriate responsiveness
- Head/neck – shape, fontanels, evidence of injury, neck mobility
- Eyes – pupillary response, conjunctival hemorrhage
- ENT – TMs, congestion/coryza, blood presence, torn
- Chest/CVS – increased work of breathing, abnormal breath sounds, abnormal rhythrm, rate, auscultation findings
- Abdomen/GU – organomegaly, masses, distension, tenderness, GU abnormalities
- Extremities – muscle tone, deformity
- Neurologic – alertness, tone, reflexes, movement and strength symmetry
- Skin – color, perfusion, bruising, erythema
BRUE CLASSIFICATION
- It is determined that a patient had a BRUE, now the patient can be categorized as either low risk or high risk.
- If the patient does not meet low risk criteria, then by default they are High Risk!
- Low Risk criteria:
- Older than 60 days
- Gestational Age 32 weeks or greaterand a Postconceptional Age of 45 weeks or greater.
- First BRUE
- Not requiring CPRby a trained medical provider
- NO concerning historic features; history concerning for potential abuse, family historyof sudden death in first degree relatives, previous Child Protective Services or Law Enforcement involvement
- NO concerning physical examination findings; Remember to do a good genital exam and look for signs of abuse!
A Patient with a possible BRUE arrives, what do you do next?
Triage Acuity
- Medical Stabilization as needed; ABC’s
- History and Physical;
- Abnormal vital sings? NOT a BRUE
- H&P meets BRUE criteria, and no other explanation found; BRUE!
- Risk Stratify
- Does the patient fit Lower Risk criteria?
- Yes: Lower Risk
- No: High Risk
- Does the patient fit Lower Risk criteria?
Disposition
High Risk:
-
- No AAP guidelines for management of high risk infants
- Consider broad differential, manage accordingly
- Hospitaliz
Low Risk:
Strong Recommendation:
-
- Educate caregivers about BRUE
- Use shared decision making to guide disposition; If family is comfortable and patient able to have follow up in 12-24 hours then may discharge to home
- Do not order unnecessary tests or treatments; CBC, CMP, CXR, CSF, ECHO, EEG, GERD Studies, home apnea monitoring, Acid suppression therapy, anti-epileptics…
- Weak Recommendations:
- Monitor patient in emergency department for 1-4 hours with serial exams and continuous pulse ox monitoring
- 12 lead ECG
- Pertussis testing
- Avoid hospitalization solely for cardiopulmonary monitoring
AAP Flowsheet

References:
- Tieder, J. S., Bonkowsky, J. L., Etzel, R. A., Franklin, W. H., Gremse, D. A., Herman, B., . . . Smith, M. B. (2016, April 25). Brief Resolved Unexplained Events (Formerly Apparent Life-Threatening Events) and Evaluation of Lower-Risk Infants. Retrieved from http://pediatrics.aappublications.org/content/early/2016/04/21/peds.2016-0590
- (2017, July 24). Retrieved from http://pedemmorsels.com/brue/
- (n.d.). Retrieved from https://www.aliem.com/2017/02/pem-brief-resolved-unexplained-event-brue/brue/
Pediatric Pearl – June 2018
Diabetic Ketoacidosis (DKA) in the Pediatric Patient
By: Hima Khamar, PGY2
Goals of Treating a Patient with DKA
- Correct Dehydration
- Correct Ketoacidosis
- Normalize Blood Sugar
- Avoid Complications
- Treat Precipitating Event
What defines DKA?
Hyperglycemia à glucose >200mg/dL
Ketosis à presence of ketones in urine
Acidosis à pH <7.3 OR HCO3 <15 mmol/L
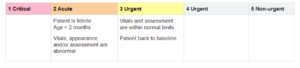
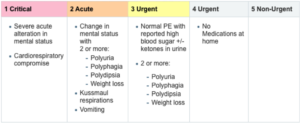
Triage/Severity Level
Critical Actions for Hour 1
1. Assess
– ABCs, VS, level of dehydration
– Mental status, neuro exam, GCS
– Risk for cerebral edema
– Monitor, VS q15 mins, I/O q 1 hr
2. IV Access
– 2 PIVs
3. Initial Labs
– POC glucose, blood or urine for ketones
– VBG, CBC, BMP, Ca, Mg, PO4, CBC, HbA1C
4. IV Fluids
– NS at 10 mL/kg
HISTORY
- New Diagnosis
- Polyphagia, polydypsia, polyuria
- Weight loss, anorexia, vomiting
- Fatigue, malaise
- Known Diagnosis
- Insulin use, most recent dose, insulin pump
- Home glucose level
- Home urine ketones
- Type DM and age at diagnosis
- Previous hospitalizations
- Previous episodes of DKA
- Hydration Status
- PO intake, UO
- Vomiting, nausea
- Infectious Symptoms
- Ingestions
- Trauma
- For Post-pubertal Female: Riks for Pregnancy, STI
PHYSICAL EXAM
- VS, ABCs, mental status (drowsy, lethargic, obtunded, coma)
- Breathing, tachypnea, Kussmaul respirations
- Perfusion: capillary refill, pulses, temperature
- Neuro exam: pupils, CN, motor, GCS
REHYDRATION
Initial fluid resuscitation
- Bolus 10 ml/kg of NS, then initiate two bag system discussed below
Maintenance fluids
- After initial bolus, begin 1.5-2x maintenance with NS with additional electrolytes as needed
- How to calculate maintenance cc/hr, use patient’s weight in kg OR just use MD calc:
- 4 mL/kg for the first 10 kg + 2 mL/kg for the next 10 kg + 1 mL/kg for each kg over 20 kg
- So for a 30 kg child, 40cc + 20cc + 10cc = 70cc/hr maintenance
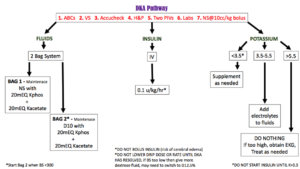
ELECTROLYTES
| Sodium | – Typically low initially due to urinary losses and fluid shift to extracellular space due to high serum osmolality
– Na correct = Na measured + (1.6 x [(glucose – 100)/100]) |
| Potassium | – May be low, normal or high, but total body stores are low due to renal losses
– <3.5, supplement before starting insulin – 3.5-5.5, add K to the maintenance fluids – >5.5, do nothing; if too high then may need to correct |
| Bicarbonate | – May be low, normal or high, but total body stores are low due to renal losses |
| BUN, Creatinine | – Elevated due to dehydration |
| Magnesium | – Low due to renal losses, replace as needed |
| Phosphorus | – Low due to renal losses, replace as needed |
NORMALIZE BLOOD SUGAR & CORRECT ACIDOSIS
Insulin
- Initiate regular insulin at rate of 0.1 u/kg/hr one hour AFTER the start of the fluid resuscitation
- Do not use insulin bolus (increases risk of cerebral edema)
Glucose
-
- Aim to lower glucose 50-100 mg/dL per hour
- Use the “two bag” system
- Bag #1: NS with electrolytes
- Bag #2: D10NS with electrolytes
- Begin dextrose bag 2 when glucose is < 300 mg/dL
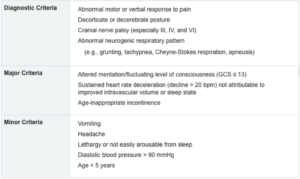
CEREBRAL EDEMA
- Leading cause of morbidity and mortality in DKA
- Etiology unclear, attributed to fluids shifts in the setting of cellular osmolar imbalance resulting in cerebral hypoperfusion and prolonged acidosis with ischemia
- Typically occurs 4-12 hours after treatment is initiated
- May be present before treatment, or occur as late as 24-48 hours after treatment initiated
Risk factors
-
- Age < 3 years
- Prior history of DKA
- pH < 7.0
- Failure of corrected Na to fall to normal range during treatment
- Administration of bicarbonate therapy
- Elevated BUN at presentation
- Low PaCO2 levels at presentation
- Administration of insulin (bolus or infusion) in first hour of fluid treatment
- Initial glucose > 1000 mg/dL
Diagnosis
MONITOR
- BS Q1H
- neuro status Q1H
- SMA7 with acetone level Q4HMONITOR
-
-
- BS Q1H
- neuro status Q1H
- SMA7 with acetone level Q4H
-
-
Pediatric Pearl – May 2018
PEDIATRIC INTUBATION
By: Dr. Lani Mendelson PGY3
HOW DO PEDIATRIC AIRWAYS DIFFER FROM ADULT AIRWAYS?
- Airway diameter = smaller
- Small diameter of airways results in higher resistance to air flow and increased chance of airway obstruction
- Airway edema results in proportionately greater obstruction
- Mandible = smaller
- Head = larger
- Neck = already in flexed position so add towels under shoulder to bring neck in neutral position
- Tongue = larger in comparison to head
- Larynx = funnel shaped larynx with anterior angulation
- Epiglottis = long, floppy, and u-shaped
- Vocal cords = angled, pink not white (harder to spot)
- Cricoid cartilage = narrowest portion, rather than the vocal cords
- Trachea = highly compliant (risks ‘kinking’)
- Short and in line with right bronchus
LARYNGOSCOPE SIZE
| AGE | SIZE |
| Premie/newborn | Miller 0 |
| 1 month – 2 years | Miller 1 or 1.5 |
| 3-6 years | Miller 2, Mac 1 |
| 6-12 years | Miller 2, Mac 2-3 |
| >12 years | Mac 3 |
*The Miller is recommended due to the more anterior airway and the floppy epiglottis of the child and infant. For a child older than 6 years of age, both Mac and Miller can be used.
ENDOTRACHEAL TUBE SIZE
Uncuffed ETT = (AGE/4) + 4
Cuffed ETT = (AGE/4) + 3.5
*If in doubt, use a tube that fits through the nose
*Premie size 3, newborn size 3.5
ENDOTRACHEAL TUBE DEPTH
ETT size x 3
AGE/2 + 12
MEDICATIONS
Atropine – not routinely recommended
- Infants and children can develop bradycardia from medication effects (especially succinylcholine), vagal stimulation of the hypopharynx/epiglottis, and hypoxia
- Should be considered in:
- 1) all patients <1 year of age
- 2) children <5 years of age receiving succinylcholine
- 3) adolescents receiving a second dose of succinylcholine (max does 1mg)
- 4) patients who are experiencing bradycardia prior to intubation
- Atropine should be given 1-2 minutes prior to any sedative or paralytic agent
Etomidate
- Sedative used most commonly for patients with hypotension or head trauma
- Risks: adrenocortical suppression hence consider a different agent in sepsis
Ketamine
- Sedative used most commonly for patients with hypotension or severe asthma
- Risks: tachycardia, hypertension, laryngospasm, and excessive salivation
Propofol
- Sedative for status epilepticus or head trauma/increased intracranial pressure
- Not recommended for < 3 years old secondary to decreased clearance
- Risks: hypotension
Benzodiazepines
- Sedative for status epilepticus
- Risks: hypotension
Succinylcholine
- Shorter duration of action
- Risks: Higher risk of malignant hyperthermia compared to other paralytics, hyperkalemia, congenital neuromuscular disorders
Rocuronium
- Longer duration of action
Benzodiazepines (midazolam, lorazepam), ketamine, dexmedetomidine, propofol, and opiates (fentanyl, morphine) are commonly used for post-intubation sedation/analgesia regimens
GO BACK TO THE BASICS. REMEMBER TO HAVE ALL YOUR BACK UPS READY.
- Positioning
- Remember necks tend to be flexed in neutral flat position (especially in those <8 yrs)
- Place towel or sheet beneath shoulders to align external auditory canal with sternal notch
- Have nasal and oral airways of the appropriate size ready
- Pre-oxygenation
- Same as adults. Use your nasal cannula for apneic oxygenation. Use NRB if needed as well.
- Would be amazing if have high flow nasal cannula available throughout intubation to prevent desaturations and prolong safe apneic times, but this is not a requirement
- May need to give some slight sedation for a fussy child with versed or Ativan to allow for pre-oxygenation
- Have suction ready
- Have BVM ready with the right size mask
- Jaw thrust can help with displacing the tongue along with aligning airways
- If you can’t remember dosing, remember the Broselow Tape
- Can’t see the cords, you may have inserted the blade or scope too far, pull back slowly; also remember they maybe pink and not white so harder to identify
- Post-intubation remember to ensure tube is not too deep
- Confirm using color change, bilateral breath sounds, US, CXR
Would you like to get more information? click here to learn about North Raleigh Pediatrics Providers.
