Lower abdominal pain in women can be challenging diagnostic dilemma in the Emergency Department. We had a case of a 50-year-old woman that had been previously seen by her PMD 3 days prior and diagnosed with a “small kidney stone” without any imaging, but did get the ever-reliable percocet prescription. Needless to say, she came to the ED because her pain wasn’t getting any better and now she was having increasing lower abdominal pain with high fevers. In the ED she was febrile (T: 104.5) and tachycardic (HR: 120s), but her BP was normal. She ended up having a WBC: 17k/mm3, bands: 20% and a pretty nasty UTI. Her pain persisted and we ended up doing a CT abd/pelvis with contrast to see if she had anything brewing. From the images below you can see that she had bilateral tubo-ovarian abscesses causing bilateral hydronephrosis seen on CT and confirmed with ultrasound. She was started on ampicillin, clindamycin and gentamicin and her abscesses were drained with CT guidance, yielding 400cc of thick, brown, purulent fluid. Yum
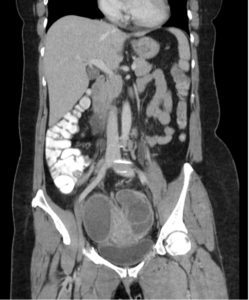
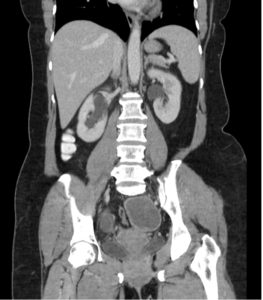
Up to one half of all cases of tubo-ovarian abscesses occur in patients with a history of pelvic inflammatory disease (PID). The theoretical etiology of tubo-ovarian abscesses is thought to revolve around an ascending infection arising in the lower reproductive tract, into the uterus and subsequently the fallopian tubes and ovaries. While Neisseria gonorrhea and Chlamydia trachomatis are commonly associated with PID, TOAs are typically polymicrobial and rarely grow either chlamydia or gonorrhea when cultured. As with most pelvic pathology, ultrasound remains the initial diagnostic modality of choice for tubo-ovarian abscesses to best visualize the upper reproductive tract. Ultrasound remains very specific (86-98%), whereas the sensitivity ranges between 56-93%. There is evidence however that computed tomography of the pelvis with contrast may provide better sensitivity than ultrasound in evaluation of TOAs. In the Emergency Department, a triple coverage antibiotic regimen (i.e. ampicillin/clindamycin/gentamicin) should be initiated despite whether the patient is going to need surgical exploration, percutaneous abscess drainage or conservative management. If the patient’s clinical status has either worsened or not improved after 48-72 hours the gynecologist will likely proceed with minimally invasive drainage procedures that have become more readily available, similar to our case.
Post by: Terrance McGovern DO, MPH (@drtmcg13)
