CC: BIB BLS for “Psych Evaluation”
HPI: 46-year-old female w/ PMH of asthma, SLE, RA and seizure disorder presents to the emergency department by BLS for evaluation. Patient states, “I don’t like people accusing me of doing things I didn’t do, I only took 2 Percocet and that’s it!” Patient states that she has been feeling depressed and “everything I do is never good enough for my kids, I buy them car, and I don’t even have car myself.” Patient appears to have multiple scratches over her face and left wrist, but is not willing to elaborate how she sustained them or provide any additional history. Denies any suicidal ideations, homicidal ideations, or hallucinations. There is no known psychiatric history.
Per family and EMS, patient was in her bedroom with the door shut, “not acting right, she was asking for us to pass her the key under the door to get out of the room but there is no lock on the door. She did this once before but it went away, today is more severe.” Pt was found in her bedroom by EMS with 2 empty beer cans and bottles of Percocet nearby. She had a recent URI for which she was taking Zzz-quil.
Medications: oxycotin 60mg q12h prn, Percocet 10/325mg q4-6h prn, toradol 10mg TID, ambien CR 12.5mg qHS, ProAir HFA 2 puffs q6h, Zzz-quil
Physical Exam:
VS: 148/101, HR 111, RR 18, T 99.1, SpO2 95% on RA
General: Awake, alert, coherent, intermittently tearful
HEENT: superficial abrasions over face, otherwise NCAT; moist mucous membranes
Eyes: 3mm PERRL
Cardiac: tachycardic, regular rhythm, no M/R/G
Lungs: CTA b/l
Abd: soft, NT, ND, normal active bowel sounds
Neuro: AAOx3, lucid, following commands, moving all 4 extremities, no gross deficits, steady gait w/o difficulty
Skin: multiple superficial abrasions over face and L wrist, normal moisture
Extremities: 2+ distal pulses, warm, normal color
Psych: Anxious appearing, depressed mood, emotionally labile, intermittently tearful; denies SI/HI
Pertinent Labs (if any)
CBC: 11.7>16.5/50.1<324
CMP (@15:09 hours): Na 135, K 4.6, Cl 106, CO2 5, Glucose 132, BUN 9, Cr 0.98, GFR >60
Alk phosphate 77, AST 59, ALT 66
UA: Moderate blood, 0-3 RBCs, occasional calcium oxalate crystals, otherwise WNL
Alcohol: <10 mg/dl
UDS: (+) cocaine
Acetaminophen: <10.0 ug/ml
Salicylate: <2.5 mg/dl
Repeat CMP (@ 17:30 hours): Na 138, K 5.4, Cl 109, CO2 <2, Glucose 143, BUN 9, Cr 1.10 GFR:53, Alk phos 77, AST 69, ALT 74
Serum Osmolality: 334 mOsm/kg (N: 283-299)
Calculated osmolar gap: 53.0 mOsm/kg
ABG: pH 7.00 / pCO2 13 / pO2 151 / HCO3 – 3.2
ABG Lactate: 20.0 mmol/L
Serum lactic acid: 1.2 mmol/L
Acetone: Negative
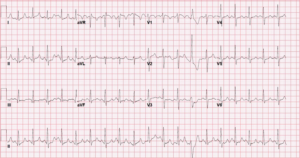
ECG in the ED
Working Diagnosis: Anion gap metabolic acidosis, most likely due to ethylene glycol poisoning
ED/Hospital course: In the ED patient became increasingly altered. Upon arrival patient was coherent, AAOx3, tearful. Upon reevaluation she was found in room shaking back and forth talking to herself and banging her hands on the bed rails, more confused, inappropriate in her thoughts and actions. A short time later she was found on the floor next to stretcher and was AAOx1, agitated, combative, not following commands, fighting with staff, incontinent of urine. Lab results returned at this time and the patient was subsequently intubated, received 1 amp sodium bicarbonate prior to intubation and admitted to MICU. Repeat labs in MICU showed persistent anion gap metabolic acidosis with Bicarbonate of 5 and anion gap of 26. She was placed on bicarbonate drip and received emergent HD. After HD, the acidosis improved with a bicarbonate value of 19 afterwards. Additionally placed on fomepizole. Received 2 rounds of HD. Subsequently extubated and transferred to floor. Upon extubation she continued to deny any SI or toxic ingestion. Methanol and ethylene glycol levels (-), however, they were drawn after HD was performed.
Pearls: Brief differential diagnosis of anion gap metabolic acidosis:
- Methanol, metformin
- Uremia
- Diabetic or alcoholic ketoacidosis
- Paraldehyde
- Isoniazid, Iron, Inhalants (carbon monoxide, cyanide, hydrogen sulfide)
- Lactic acid
- Ethylene glycol (ethanol may produce a small gap)
- Salicylates, solvents
Osmolar gap:
- Calculated osmolar gap ≥10 is consistent with poisoning by alcohols (ethanol, methanol, ethylene glycol, isopropanol, propylene glycol), glycerol or mannitol
- Absence of osmolar gap does not exclude toxic alcohol poisoning.
- Normal osmolar gap: ±10
- Normal serum osmolality: 280-295 mOsm
- Osmolar gap formula: (2 x Na) + BUN/2.8 + Glucose/18 + Ethanol/4.6
- Labs for this calculation (i.e. serum osmolality, ethanol, and SMA-7) must be drawn at the same time for accuracy
Toxic Alcohol Poisonings:
- Methanol
- Found in windshield washing fluids, solvents, paint thinners and canned fuels
- Converted by alcohol dehydrogenase to formaldehyde then to formic acid
- Accumulation of formic acid correlates with the decrease in bicarbonate, the increase in anion gap, and the severity of the metabolic acidosis
- Formic acid affects optic nerve function, causing optic papillitis and retinal edemaà “blind drunk”
- Visual symptoms include photophobia, “snowstorm” vision, and blindness
- Management:
- Supportive measures including airway management
- Severe acidosis is treated with bicarbonate to reduce diffusion of formate into the CNS and protect the optic nerve
- Alcohol dehydrogenase inhibitor (ethanol or fomepizole) to block further metabolism of methanol
- Fomepizole Fomepizole (4-methylpyrazole) is preferred iv.
- Hemodialysis to remove methanol and formic acid indicated if methanol level >50 mg/dL, metabolic acidosis (arterial pH ≤ 7.25), severe visual or CNS symptoms
- Management:
- Ethylene glycol
- Found in antifreeze and brake fluids
- Converted by alcohol dehydrogenase to glycolaldehyde which is metabolized to glycolic acid
- Glycolic acid is primarily responsible for the anion gap metabolic acidosis; it is metabolized to multiple metabolites including oxalic acid
- Oxalic acid forms calcium oxalate crystals in the kidney, brain and liver
- Initial CNS changes suggestive of ethanol intoxication progressing over 9-12 hours to possible seizures, stupor, coma; toxicity may progress to pulmonary edema and myocardial dysfunction
- Late toxicity is characterized by renal failure
- Positive birefringent calcium oxalate crystals in the urine; often absent initially commonly described as “envelope-shaped”
- May see hypocalcemia although not always present
- Management:
- Alcohol dehydrogenase inhibitors: Fomepizole or ethanol
- Hemodialysis with same indications as methanol above
- Thiamine and pyridoxine can be administered to decrease production of oxalic acid
-
- Isopropanol
- Isopropyl (rubbing) alcohol
- More intoxication/CNS depression but generally less severe sequlae than methanol and ethylene glycol 80% is absorbed from the stomach within 30 minutes and metabolized by alcohol dehydrogenase to acetone
- Presentation: CNS depression, hypotension in severe cases, hemorrhagic gastritis/tracheobronchitis
- Positive serum acetone and acetonuria
- Anion gap metabolic acidosis is generally not a feature of isopropanol toxicity (unless you have significant hypotension with subsequent lactic acidosis)
- Management:
- Supportive care, including airway management
- Alcohol dehydrogenase inhibitors are not indicated
- Hemodialysis indicated for refractory hypotension or serum levels >400-500 mg/dL
Some Additional Points:
-
-
- Lactic acid on lab analysis may be falsely elevated and vary depending on how the sample is analyzed. You will note that ABG lactic acid and serum lactic acid analyzed by lab are very different values, this is due to the fact that a metabolite of ethylene glycol’s metabolism has a very similar chemical structure to lactic acid, causing a falsely positive elevated lactic acid
- The differential diagnosis of anion gap metabolic acidosis listed above is a limited list of the most commonly noted causes of AG metabolic acidosis; a comprehensive list is much broader
- An osmolar gap >50 is highly suggestive of toxic alcohol ingestion; a level >100 is virtually pathognomonic—there is really nothing else that can cause such a severely elevated osmolar gap other than toxic alcohol
-
Case presented by Dr. GregnCassidy
Special thanks to Dr. Kashani for his guidance in preparing this case.
