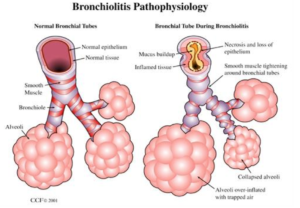
Pathophysiology
- Disorder that is commonly caused by a viral lower respiratory tract infection in infants
- Characterized by acute inflammation, edema and necrosis of epithelial cells lining small airways and increased mucus production
- Etiology
- Coronavirus
- Influenza
- Rhino virus
- Adenovirus
- Parainfluenza virus
- RSV (respiratory syncytial virus) – MOST COMMON!
- Incidence – December-March
-
- Most infections occur within first 2 years of life
- About 40% experience lower respiratory infection during initial infection
- RSV doesn’t grant permanent or long-term immunity – RE-INFECTION COMMON
- The risk of significant viral or bacterial lower respiratory tract infection or pneumonia in an infant is low
-
- Transmission
- Direct contact with secretions
- Young children shed virus for >2 weeks
- 30-70% of household contacts become ill
- Natural history
- Begins with URI – Rhinorrhea, congestion, cough
- Progresses to LRI in 2-6 days – Airway obstruction (tachypnea, wheezing, respiratory distress)
- Variable and dynamic course
- Lasts 2-4 weeks
Case

7-month-old male presents to the emergency room with his parents due to cough, runny nose, congestion and SOB that started 3 days ago.
VS: RR – 65, HR – 140, Temp – 99.1°F, O2 sat – 93% on RA
History
- Typical Presentation of Bronchiolitis
- Viral URI and cough with signs of lower respiratory tract infection
- Work of breathing – grunting, nasal flaring, intercostal/subcostal retractions
- Tachypnea
- Wheeze
- Coarse rales
- Viral URI and cough with signs of lower respiratory tract infection
Physical Exam
- TIPS for a better exam
- Upper airway obstruction can contribute to work of breathing
- Suctioning and positioning may decrease the work of breathing and improve the quality of your examination
- Counting respiratory rate over the course of 1 min is more accurate than shorter observations
- Assess mental status, respiratory rate, work of breathing, oxygen status, listen to breath sounds, and assess hydration status
Diagnosis
- DIAGNOSIS IS CLINICAL – NO LABS OR RADIOLOGICIAL STUDIES ARE NEEDED
- When to consider CXR – if child has had >2 days of fever, an asymmetric chest exam, does not demonstrate improvement or has an unusually high O2 need
- Diagnostic testing may be considered if:
- Need cohorting – this is why we get testing for those we admit
- Uncertain clinical diagnosis
- Age <2 months
- To assess for influenza – also needed this for those we admit
Management
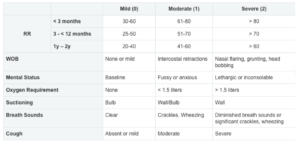
Classify patient as mild, moderate, or severe based on the above physical exam
| Mild | Moderate | Severe |
| 1. Consider suction bulb
2. Discharge |
1. Suction bulb
2. No bronchodilators 3. Discharge or admit |
1. Suction bulb or wall
2. No bronchodilators 3. If no improvement consider starting high flow NC 4. Admit |
- Rehydration
- IVF – moderately or severely dehydrated, secretions are thick and difficult to mobilize or severe respiratory distress
- PO feeds – mildly to moderately dehydrated and can tolerate PO
- Considerations for severely ill patients
- Consider ONE TIME albuterol MDI trial if:
- Severe respiratory distress OR
- Increased risk for asthma
- >12 months old, wheeze and once of the following
- personal history of atopy or recurrent wheezing
- strong family history of atopy or asthma
- if responds to albuterol then consider switching to asthma pathway
- >12 months old, wheeze and once of the following
- Consider HFNC for significant hypoxia OR severe respiratory distress not improving with rigorous supportive care
- Consider ONE TIME albuterol MDI trial if:
| Discharge criteria | Admission criteria |
| – Oxygen saturation >90%
– Awake – Adequate oral intake – Mild/moderate work of breathing – Reliable caretaker – Able to obtain follow up care – MDI/spacer teaching if response to albuterol |
– Admit if discharge criteria not met:
o Inpatient: Requires 02 or progression expected o OBS: Mild disease with expected LOS < 24 hours o ICU: Apnea, severe distress; Requires HFNC / CPAP / intubation – Infants with these risk factors present early in the illness have higher risk of progression: o Gestational age < 34 weeks o Respiratory rate ≥ 70 o Age < 3 months |
Additional Notes
- Differentiate infants with probable viral bronchiolitis from those with other disorders
- The above management points to do take into consideration patients with significant medical history such as congenital heart disease, anatomic airway defects, neuromuscular disease, immunodeficiency, chronic lung disease – ADMIT, HIGH RISK!
- The physical exam will vary from minute to minute depending on child’s position, level of alertness, response to treatment – CONSTANTLY RE-EVALUATE!
- If patient presents within the first couple of days, they may worsen and need admission at a later point – PARENT EDUCATION IS KEY!
- Viral illness, treated by hydration and suction
- Signs of respiratory distress
- How to suction
- When to suction
- Frequent feeds and watch hydration status
- Cough may last 2-4 weeks, do not use OTC cough and cold medications
- Avoid tobacco smoke
- NOT RECOMMENDED!
- Albuterol – Wheezing is due to the airways being clogged with debris not bronchospasm
- Racemic epinephrine
- Corticosteroids
- Chest physiotherapy
- Montelukast
- Antibiotics
- Hypertonic Saline
- Routine testing
- Chest X-rays
References
- http://pediatrics.aappublications.org/content/134/5/e1474
- http://www.chop.edu/clinical-pathway/bronchiolitis-emergent-evaluation-clinical-pathway
- http://www.cochrane.org/CD001266/ARI_bronchodilators-for-bronchiolitis-for-infants-with-first-time-wheezing
- http://www.seattlechildrens.org/healthcare-professionals/gateway/pathways/
Special thanks to Dr. Hima Khamar, MD PGY-2 for her contribution to this month’s Pediatric Pearls!
