Case of the Week COW#13
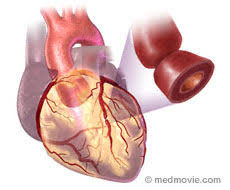
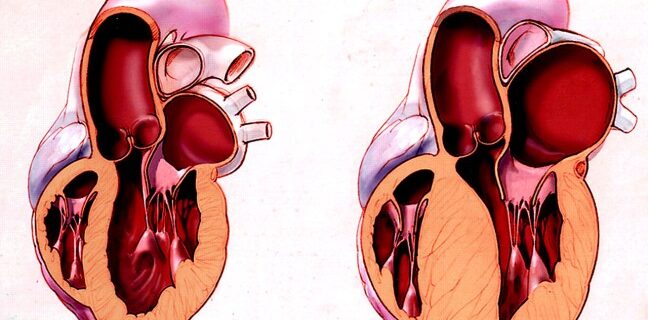
CC: Chest Pain HPI: 49-year-old female brought in via ALS presents complaining of Chest pain. As per the Paramedics, the patient was found to be in no acute distress, stating she had exertional chest pain, which had subsided. The pre-hospital ECG was suspicious for ischemia and she was given ASA. Patient states she was walking home …