CC: Left leg pain
HPI: 52 year old male with PMH of IDDM presents to the Emergency Dept. (ED) with left leg pain for the past 9 days which has become progressively worse. He is a taxi driver and reports that a part of the seat, which supports his legs, has been rubbing against his left hip/buttock/thigh and he thinks this is what’s causing the pain. He reports pain to the back of his left buttock, which radiates down the leg “like a shooting pain.” The patient has been to the ED multiple times already for similar complaints, requesting for stronger pain medications. He is upset because he feels the medicine just isn’t working. At this point, the patient is uncooperative and refuses to answer any more questions. Further history was obtained from his previous visit history, which stated he was discharged yesterday with a diagnosis of sciatica and a prescription for Lidoderm patch, Motrin and Percocet.
PMH/Birth History: N/A
Social History: N/A, refused to answer any further questions
PHYSICAL EXAM
VS: BP 125/59 HR 108 RR18 T: 98F 98% RA
General: In moderate acute distress, appears stated age, in moderate pain, uncomfortable and diaphoretic.
HEENT: Atraumatic, normo-cephalic. No deformities. PEERLA
Respiratory: Lungs CTA bilaterally.
Cardiac: +S1/S2, no MRG, regular rate and rhythm
Abdomen: soft NT ND
Extremities: B/L DP 2+, Cap refill < 3 seconds, positive straight leg (LLE); pain isolated to (L) buttock and posterior lateral thigh.
Neuro exam: CN III –XII intact. 5/5 strength in all 4 extremities with limited ROM in the LLE secondary to pain.
Skin: Diffuse erythema over the Left buttock extending down to the posterior lateral left thigh, with pitting edema. No fluctuance or streaking noted.
Labs:
WBC: 24.7 H/H: 13.1 / 39.4 Platelets 245 PMH: 22.1 Lymph: 0.7 Mono: 1.5
Na: 126 K: 5.5 Cl: 89 CO2: 22 Glucose: 438
Bun: 38 Cr: 1.17 Alk P: 140 LFT: WNL Albumin 3.2
Acetone: NEG
ESR: 65
CRP: 30
Lactic acid: 1.4
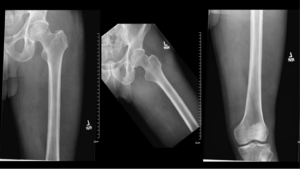
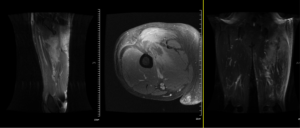
Images:

Repeat Vital Signs 139/81 89 16 99.7F 97% ON RA
MRI
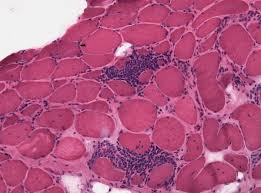
Working Differential Diagnosis: Pyomyositis
ED/Hospital course: Orthopedic Surgery was consulted. X-Ray did not show obvious bony involvement and ESR/CRP was not suggestive of osteomyelitis. MRI was performed on the LLE, which sowed a hyper-intense signal within multiple muscles of the pelvis and left thigh consistent with myositis. Collection within the Obturator Externus and Gluteus Maximus muscles likely represented an abscess consistent with pyomyositis. The patient was started on Vancomycin and Zosyn and sent to Interventional Radiology for drainage of the abscess. The cultures grew back MSSA. The left knee tap did not grow any organisms on Gram Stain. IR drainage was followed by orthopedic washout and debridement of the musculature with insertion of JP drain for continuous drainage. The patient’s antibiotics were switched to Levaquin and he was subsequently discharged home with Clindamycin and Bactrim for 2 more weeks. He tested negative for HIV.
Pearls & Takeaways:
- Don’t blow off patient’s complaints! Our patient presented with History and Physical exam consistent with sciatica with a positive straight leg test. He was on Percocet and kept asking for stronger medications for his previously diagnosed Sciatica.
- Make sure to undress the patient and examine the skin!
- If the patient is complaining of pain out of proportion to his/her exam, dig a little deeper for alternative differential!
- Since his Accucheck was High, further laboratory testing was done which revealed leukocytosis. The elevated white count prompted me to perform a further work up
- Always re-evaluate the patient! On re-evaluation, he appeared sicker and with cool, damp skin on his back and neck, solidifying my gestalt that maybe I am missing something
- Pyomyositis is a purulent infection of skeletal muscle that arises from hematogenous spread, usually with abscess formation.
- Risk Factors: immunodeficiency (HIV).
- auerus is the most common cause of pyomyositis; it causes up to 75 – 90% of cases.
- Pyomyositis presents with fever and pain and cramping localized to a single muscle group. It develops most often in the lower extremity (sites include the thigh, calf and gluteal muscles) but any group of muscles can be involved including iliopsoas, pelvic, trunk, Paraspinal and upper extremities.
- MRI is the most useful imaging modality for diagnosing the disease. It can distinguish the defining sites of infection and rule out other entities.
- Nonspecific lab findings include Leukocytosis and elevated inflammatory markers but CPK are often normal.
- Empiric antibiotics should be directed against Staph/Strep for immunocompetent. Immunocompromised should be covered for Gram negative, gram positive and anaerobic organisms should be considered.
- Pyomyositis is graded based on stages.
- Stage 1 (Invasive stage, 1-2 weeks, may only have pain) can be treated with Antibiotics alone.
- Most patients present with Stage 2 (Suppurative stage, weeks 3-4)
- Stage 3 (Late stage) due to delay in diagnosis and usually requires drainage for definitive management.
Case presented by Dr. Michael Hong