CC: Shortness of breath
HPI: 7 day old female presents to the Emergency Dept. (ED) after being seen earlier in clinic. Mother is rom Nigeria and arrived to the U.S a few weeks prior to delivery. Prenatal care is unclear. Patient was delivered via C-Section at 39 weeks at another nearby hospital. Both mother and baby spent one day in the hospital after delivery being discharged home. Mother states that since last night, the baby appears to “ not breathing right.” She also hasn’t’ been eating much and is crying more often than usual, during which her lips start to turn blue.
Physical Exam:
Obvious respiratory distress, hypoxic on RA, saturating in the middle to low 80’s on NC 3 L
HR 176, RR 60. Accuchek 96.
BP: (RA) 69/45 BP (LA) 91/64 BP (LL) 84/64 BP (RL) 71/58
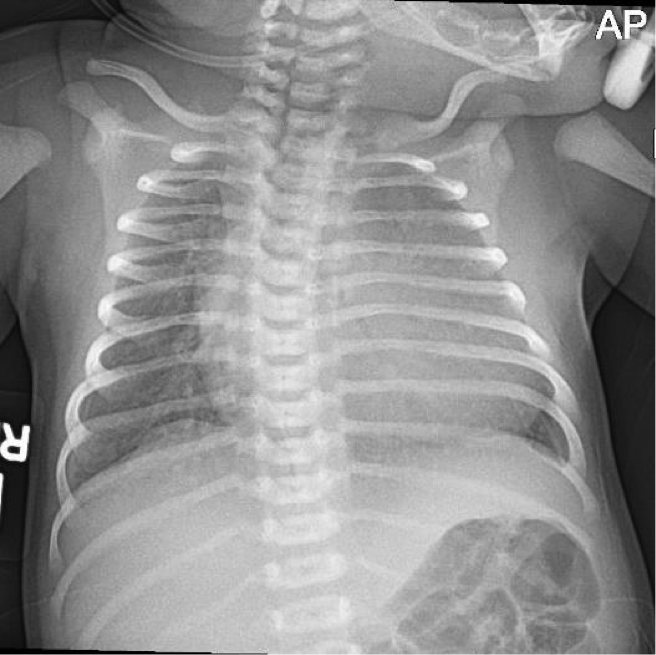
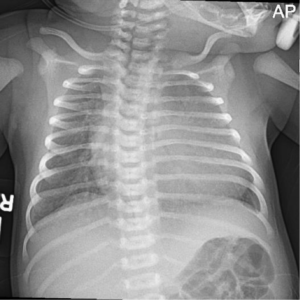
Pertinent Imaging/ECG
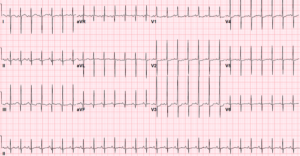
ECG in the ED:
Working Diagnosis: Shock secondary to congenital cardiac pathology.
ED/Hospital course: Patient was admitted to PICU, underwent Echocardiogram and further imaging and was diagnosed with Coarctation of the Aorta. The patient was transferred to Mt. Sinai for operative repair.
Pearls:
- 7 day olds are terrifying, especially if they are sick.
- Take a breath! Start with your ABCs.
- Coarctation of Aorta(CoA) is a congenital aortic narrowing which most commonly occurs at the level of ductus arteriosis. There are Pre-ductal and Post-ductal types. Pre-Ductal CoA is a Truncus dependent lesion and most patients present within 2 weeks of birth once duct closes. Aortic narrowing leads to increased LV function and dilation. Post-ductal are commonly identified in adulthood.
- Obtain a BP/pulse Ox in all 4 extremities
- Perform the Hyperoxia test
- Obtain ABG on RA. Then, apply 100% supplemental oxygen with a NRB for 10-15 minutes. Repeat the ABG on the NRB.
- On repeat ABG
If PaO2 > 250mmHg = Lung problem
If PaO2 < 100mmHg = Congenital Heart Disease
If PaO2 100-250: Assume the worst situation first
- On repeat ABG
- Obtain ABG on RA. Then, apply 100% supplemental oxygen with a NRB for 10-15 minutes. Repeat the ABG on the NRB.
- You may also apply supplemental oxygen and assess the infant’s response. If saturation increases to at least 5-10%, it’s most likely a Lung problem. If it remains the same, think about Congenital Heart Disease
- Prostaglandin (pt is less than 4 weeks old typically 1-2 weeks of life) start at 0.05 mcg/kg/min.
- Dr. Hochman rule #11, call consultants early “don’t be the captain of a sinking ship”
- Additional medications: Lasix 1 mg/kg if evidence of volume overload.Ductal dependent lesions, pulmonary presentation cyanosis/hypoxia use phenylephrine . If systemic SX, shock, pulmonary congestion on CXR Milrinone (decrease afterload + inotropic support).
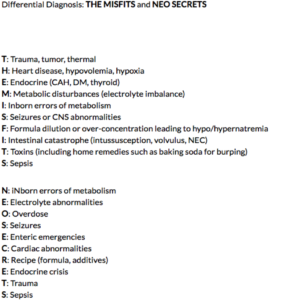
The SICK NEONATE!
Case presented by Dr. Daniel Poor