CC: Numbness and palpitations
HPI: 21-year-old Female presents to the Emergency Department (ED) complaining of palpitations and left arm weakness with perioral numbness, which began just prior to arrival. The patient states the episode lasted 30 minutes before completely resolving on its own. In the ED, she denies any other complaints except for a mild headache. Patient notefs she experienced a similar episode of palpitations yesterday afternoon, while resting, which she described as “skipping beats”. On further questioning, the patient admitted to being hospitalized to a NYC hospital 2 weeks ago where she had a Cardiac Echocardiogram done which showed “hypertrophy.” Patient never followed up with cardiologist as instructed. In the past, a doctor in her country prescribed her an unknown antihypertensive medication, which she took for one year but stopped taking it once she moved to NJ. Denies fever, dizziness, chest pain, and shortness of breath, recent travels, calf pain or swelling.
Physical Exam:
BP 109/72 HR 82 RR 18 SpO2 100% on RA Temp 97.0F
General: Well appearing female, in non-acute distress
HEENT: NCAT, pupils PERRLA, neck supple
Respiratory: CTA B/L, no wheezing, rales or rhonchi
Cardiac: +S1/S2, no MRG, regular rhythm
Abdomen: soft NT ND
Neuro exam: AAO X 3, No focal deficits
Extremities: no edema, no tenderness or swelling, 5/5 strength in all extremities. Sensory intact
Skin: pink and warm, No diaphoresis, no rashes, lacerations, or abrasions
Pertinent Labs: Troponin 0.308
Pertinent Imaging and other tests:
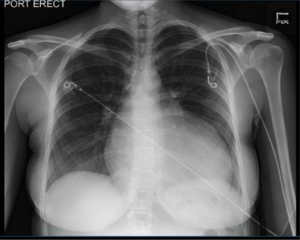
- Chest X-Ray: Cardiomegaly with a boot shaped heart, which may indicated right heart failure.
- CT Head: Normal
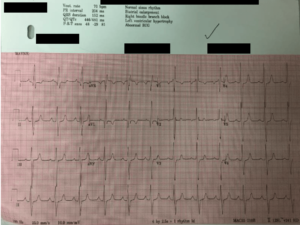
- ECG: Normal Sinus Rhythm, Bi-atrial enlargement, RBBB, LVH
Working Diagnosis: Hypertrophic Cardiomyopathy (HCOM)
ED/Hospital course: Patient was given 324 mg of ASA and admitted to Telemetry with a diagnosis of Hypertrophic Cardiomyopathy. While still in the ED waiting for a bed on Telemetry the patient had multiple runs of non-sustained V-Tach and Cardiology was consulted. The patient was started on ASA and Metoprolol PO. A 2D ECHO was done which was consistent with HCOM. Patient remained stable on Telemetry for 3 days prior to discharge. The patient’s Troponin was trended daily, 0.308 in the ED, 0.288 on day 1 of admission, and 0.314 on day 2 of admission. Patient was told by her family medicine doctor to follow up with Cardiology Clinic for possible AICD placement planning.
Pearls:
Hypertrophic cardiomyopathy (HCM) is one of the most common inherited cardiac disorders (affecting ~ 1 in 500 people) and is the number one cause of sudden cardiac death in young athletes. Annual mortality is estimated at 1-2 %.
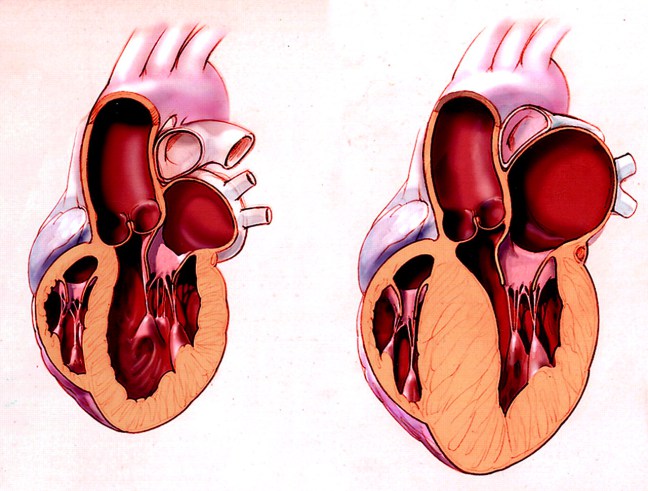
- Pathology and Pathophysiology:
- Dynamic Obstruction of the Left Ventricular Outflow Obstruction (LVOT)
- Primarily Autosomal Dominant Inheritance
- Left Ventricular diastolic dysfunction resulting from impaired relaxation and filling of the stiff and hypertrophied left ventricle (often associated with increased filling pressure)
- Abnormal intramural coronary arteries with thickened walls and narrow lumens
- Chaotic, disorganized left ventricular architecture (“ cellular disarray’) predisposing to abnormal transmission of electrical impulses and thus serving as a substrate for the formation of arrhythmia.
- Clinical Manifestation
- Exertional syncope or pre-syncope – this is the most worrisome symptom, suggesting dynamic LVOT obstruction with or without dysrhythmia, with the potential for sudden cardiac death.
- Symptoms of pulmonary congestions due to left ventricular dysfunction (e.g. exertional dyspnea, fatigue, orthopnea, paroxysmal nocturnal dyspnea)
- Chest pain – may be typical angina pain due to increased demand (thicker myocardial walls) and reduced supply (aberrant coronary arteries).
- Palpitations due to supraventricular or ventricular arrhythmias.
- ECG Features:
- Left atrial enlargement
- Left ventricular hypertrophy with associated ST segment / T-wave abnormalities
- Deep, narrow (“dagger-like”) Q waves in the Lateral (V5-6, I, aVL) and inferior (II, III, aVF) leads. Most common in Lateral vs. Inferior
- Giant precordial T-wave inversions in apical HCM
- Signs of WPW (Short PR, delta wave)
- Dysrhythmias: Atrial Fibrillation, supraventricular tachycardia, PACs, PVCs, VT
*** Infarction Q Waves are wider with a different morphology compared to HCM.
Pathologic Q Waves:
- Usually > 40 ms (1mm) wide
- > 2mm Deep
- > 25% of depth of QRS Complex
- Best seen in V1-V3