CC: Altered Mental Status
HPI: 50 -year-old Male with PMH of HIV, CVA and Meningitis presents to the Emergency Department (ED) for altered mental status. As per the patient’s girlfriend at bedside, the patient woke up confused and was not making any sense when he spoke. He even urinated on the floor but does not remember doing so. Patient had been complaining of back pain, testicular pain and leg pain for the past couple of weeks and had been evaluated for it in the ED. Patient also states he is currently taking “something for his HIV” but is unclear what his last CD4+ count was. Denies sick contacts. The rest of the review of systems was limited by confusion, but denied vomiting, diarrhea, abdominal pain, or any other complaints.
Physical Exam:
BP 128/78 HR 129 RR 14 SpO2 96% on RA Temp 102.4F
Constitutional: Diaphoretic, confused and intermittently following commands.
HEENT: NCAT, pupils PERRLA, neck supple
Respiratory: CTA B/L, no wheezing, rales or rhonchi
Cardiac: +S1/S2, tachycardia, no MRG, regular rhythm
Abdomen: soft, mildly distended with mild tenderness in RUQ and LUQ. Was not able to appreciate any focal masses . No rebound or guarding
Neuro exam: Not oriented to time or situation, No focal deficits, moving all four extremities. Unable to complete a more detailed exam as patient remained confused.
Extremities: no edema, no tenderness or swelling
Skin: pink and warm with diaphoresis, no rashes, lacerations, or abrasions
Pertinent Labs:
(Per Sorian Inpatient) CD4 = 120 on June 2017
Sepsis workup summary (normal if not reported):
- Trop 0.045ng/ml
- Sodium 126
- WBC 5.8 Chloride 93
- RBC 3.72 CO2 19
- HBG 10.3 Glucose 116
- HCT 30.3 BUN 89
- Platelets 108
- Cr 2.90 (↑ from baseline)
- Bands 27 Total Bili 4.5
- Lymphs 3 Total Protein 5.7
- Monos 2 Albumin 2.6
- Lymphocytes 0.2
- Alk Phos 346 Monocytes 0.1
- AST 143
- ALT 58
- Lactic acid 3.4
- U/A negative
- CSF negative
Pertinent Imaging and other tests:
EKG remarkable for sinus tachycardia, left axis deviation, and an old RBBB
CT head w/o contrast remarkable for only mild frontal volume loss
Chest XR – unremarkable
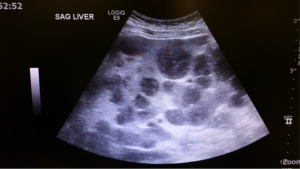
RUQ Bedside US and then official US completed and showed:

Working Diagnosis:
Hepatic hydatid cysts from Echinococcus tape worm
Hepatic abscesses
Metastatic cancer
Multiple biliary hamartomas
Polycystic liver disease
Caroli Disease
ED/Hospital course:
In the ED, the patient received IV Fluid boluses of NS 30mg/kg and one 1000mL of NS along with Tylenol, Vancomycin and Zosyn. The patient was admitted to Infectious Disease service. Throughout the hospital stay, CT Scan of abdomen and pelvis w/o contrast (due to AKI) was remarkable for infiltrated liver, splenic lesions, and destructive lesions of the bilateral iliac wings and L5 with pathologic fracture of the posterior right rib, which may be due to metastatic disease. The underlying etiology is uncertain. Without contrast, it was not certain if there was underlying macronodular cirrhosis. There was also associated ascites. Initial blood cultures from the ED grew Salmonella species. The patient was initially admitted the medical floor but was transferred to the Medical ICU on day 7 of hospitalization for increased lethargy and worsening lactic acidosis, transaminitis, and AKI. He later went into multisystem organ failure and was intubated thereafter. His code status was also changed to DNR/DNI. The patient unfortunately expired before endoscopy, colonoscopy, and biopsy could be performed.
Official Ultrasound read – Findings consistent with metastatic disease to the liver.
Pearls:
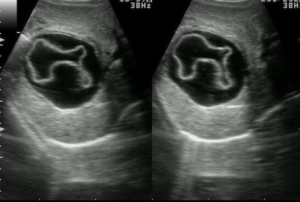
Hepatic Hydatid infection
- Caused by Echinococcus granulosus or Echinococcus multilocularis
- granulosus – Endemic in North America & Australia with dogs & wolves main as main host
- multilocularis – Found in Northern Hemisphere with red fox, dogs, & cats as main host
- Ultrasound would show a multiseptate cyst with daughter cysts
- X-ray would show calcified rings
- CT Abd/Pelvis may show the water-lily sign, which occurs when the endocystic membrane becomes detached, resulting in floating membranes within the pericyst, which mimics the appearance of a water lily ( Refer to Figure 1).
Figure 1. A detached membrane within the contents of the cyst, known as the water-lily sign
Pearls
Hepatic Hydatid infection
- Infection may be asymptomatic for many years, with a long latent period (up to 50 years of age!)
- Albendazole for confirmed infection
- Reserve antibiotics for those in which diagnosis is uncertain due to risk of anaphylaxis
- Most cases in U.S. occur in immigrants from endemic countries (South America, Middle East, eastern Mediterranean, sub Saharan, African, West China, former Soviet Union)
- Confirmed cases in U.S. are rare
Patients with HIV
- Always ask for CD4+ count and if they are on medications for their HIV/AIDs
- Have a low threshold for doing an aggressive workup for these individuals, especially if poor follow up
- HIV is a risk factor for Salmonella bacteremia
- Other risk factors include any immunosuppressed state, liver disease, hemoglobinopathies (decreased splenic function)
- Most salmonella bacteremia can have a preceding diarrheal illness
- Major complication is endovascular infection
- Treatment is IV fluoroquinolones or 3rd generation cephalosporin
Case presented by Jessica Williams, MD, PGY1