Case of the week COW #10
CC: Nausea and vomiting and “ I think my sugar is low” HPI: 36-year-old Female with PMH of Diabetes presents to the Emergency Department complaining of multiple episodes of non-bloody, non-bilious vomiting for the past 5 days. Associated symptoms include chills and a mild sore throat. Denies fever, HA, neck pain, chest pain, SOB, abdominal …
ACEP Now Review on LVADs
Check out this excellent review on managing patients with LVADs from this month’s ACEP Now publication which was written by our own Dr. Yenisleidy Paez Perez, DO PGY-3 and one of our newly graduated residents, Dr. Terrance McGovern, DO.
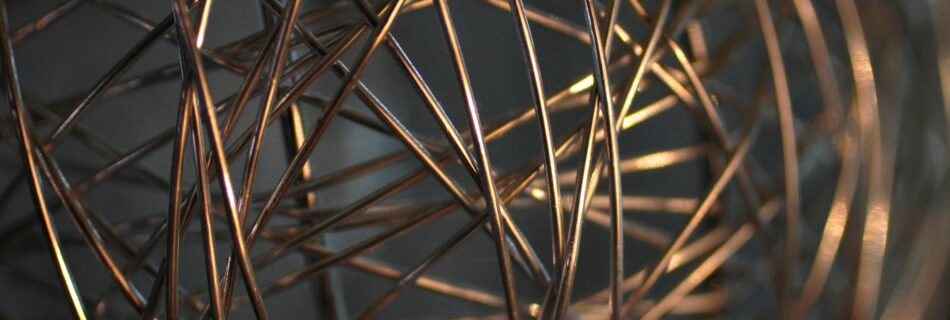
TLC: Triple Lumen Complications
Placing central venous cathethers, whether under ultrasound guidance or based off of your landmarks can be difficult and still prone to many complications. With the increased use and now standard of care for placing central lines with ultrasound guidance you would think we are immune to the “catastrophic” complication of an inadvertent arterial cannulation. But does ultrasound make us infalliable? Are there other methods that we can use to confirm venous placement of these large catheters?
Blunt chest trauma
Being in a car accident, even the most benign one imaginable, can be stressful for patients. Inherently, if they have any chest pain they’re going to be convinced they’ve sheared their aorta right off its hinges. While that may be of concern to them, we are pretty certain that their aorta is still intact if they still are alive, but did they sustain a cardiac contusion? How do we even figure out if they had one? And what the heck do we do with them if they did in fact have a cardiac contusion?
Time for Terlipressin?
Correct, we don’t have terlipressin in the US, yet… Hopefully, sometime in the not so far off future we’ll have the chance to play around with it. Essentially it’s a synthetic analog of vasopressin which we are more familiar with. There’s some written about its use in variceal bleeds and here is a cool little study from Egypt using it for refractory septic shock.
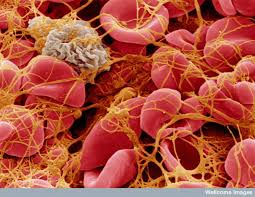
Stressed vs unstressed volume
Dr. Rory Spiegel, from EMNerd, wrote a recent piece in Clinical and Experimental Emergency Medicine about how our undying love for left ventricular function in shock patients is perhaps overdoing it and the focus should rather be on the venous return.