|
Presenting Resident |
Traficante |
|
Chief Complaint |
Cardiac arrest |
|
Brief HPI |
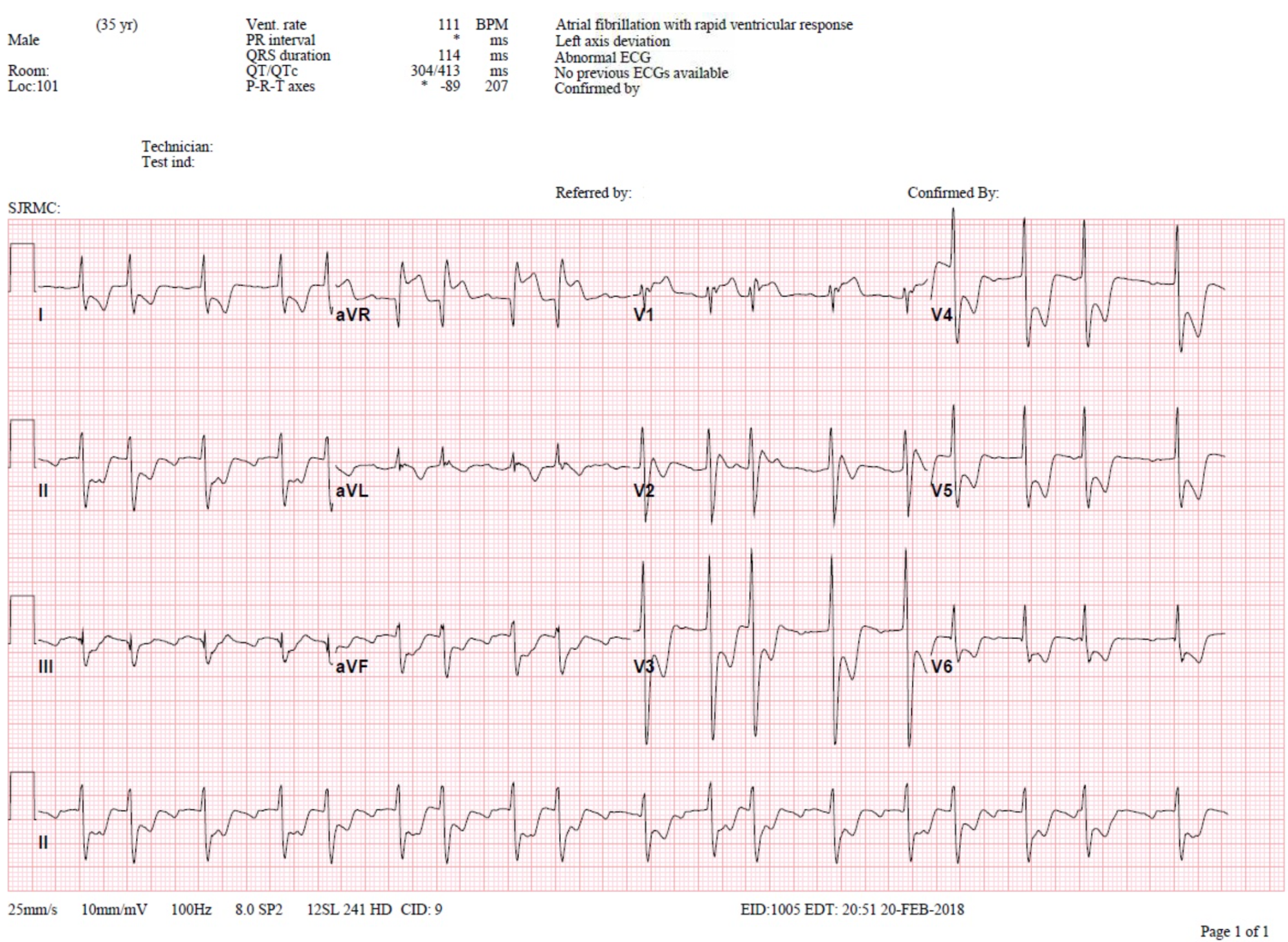
Hispanic male in his mid 30s who presented to the ED as John Doe after he was found unresponsive in the field with cardiac arrest. Unknown downtime. As per EMS endorsement from bystanders, the patient allegedly had a witnessed syncopal episode followed by seizure-like activity after which he became unresponsive. No bystander CPR. EMS arrived at the scene and found him pulseless, CPR started. On ALS arrival patient found to be in PEA. CPR, intubated, epi x 2, bicarb then ROSC achieved. Initial rhythm in ED was sinus tach on monitor. After 5 min in ED patient became bradycardic and went into PEA, compressions started, received epi x 1 w ROSC. Pt then went into wide complex tachycardia on monitor – SVT vs Vtach – pt was cardioverted 200J and given Amiodarone 150mg. Post cardioversion, rhythm changed to afib v aflutter. EKG was obtained after 10 min (below). |
|
Pertinent PE and Vitals |
On arrival: BP 81/50; P113; SpO2 95% ambubag 100% FiO2; Temp 37.0; BS 136 PE: On admission: BP 153/83; P153; SpO2 98% on vent 100% FiO2 |
|
Pertinent Labs |
ABG done on patient arrival = 6.80/86/253/14; Na+ 133; K+ 4.4, Ca++ 1.04; Glu 246, Lac 8.8, BE -10.2 These were the only labs available at the time of admission. |
|
Pertinent Imaging/EKG |
|
Working Diagnosis at time of Disposition |
Cardiac Arrest |
|
ED & Hospital Course |
Interventional cardiologist advised immediate transfer to cath lab for diagnostic cath (did not want to wait for CT Head). Cath showed normal coronaries with LVEF 75%. Patient transferred to the CCU post cath. He was noted to have no brainstem reflexes off sedation. CT Head showed findings c/w anoxic encephalopathy, no bleed. Neuro was consulted who stated patient’s exams and further diagnostic studies were significant for loss of all cortical and brain stem function, consistent with brain death. Patient was pronounced on Day 10 (delay with identifying patient and determining NOK). |
|
Pearls & Takeaways |
Is ST-Segment Elevation in Lead aVR Getting Too Much Respect? Introduction ECG reading is all about pattern recognition. And this particular pattern of ST-Elevation in aVR with diffuse ST Depression is a very important ECG pattern that you must be able to recognize. But what’s probably more important than being able to recognize the pattern, is understanding what it represents. There appears to be a common misconception that the ST-Elevation in aVR always represents “STEMI”, or acute transmural (full- thickness) ischemia. If this were the case the patient would most likely be dead or at the very least in profound cardiogenic shock. The key to understanding what this pattern represents lies in understanding that the ST-Elevation in aVR is reciprocal to the diffuse ST-Depression – and that this diffuse ST-Depression represents global subendocardial ischemia. So the real question that you must answer is: What is causing the global subendocardial ischemia? What Else can Cause STE in aVR that Won’t Benefit from Going to the Cath Lab? Worrisome Diagnoses:
Non-Worrisome Diagnoses:
It is critical to realize that more often than not the cause is global myocardial strain from a Non-ACS etiology! (profound sepsis, tachycardia, anemia, hypoxemia, etc). In our patient above it may have been because of the SVT he was in during the code in addition to being in Afib w/ RVR at the time of the ECG. It is also very important to understand that in these Non-ACS settings, you can see this pattern with or without underlying coronary artery disease. But of course it could be ACS. And if it is, then you are dealing with Left Main, Proximal LAD, or even multi-vessel plaque instability. But keep in mind that even if it is ACS you are still dealing with subendocardial and not transmural ischemia. Take Home Points
|
References: http://hqmeded-ecg.blogspot.com/2018/02/st-elevation-in-avr-with-diffuse-st.html